Pancreatitis – What It Is and Why It Matters
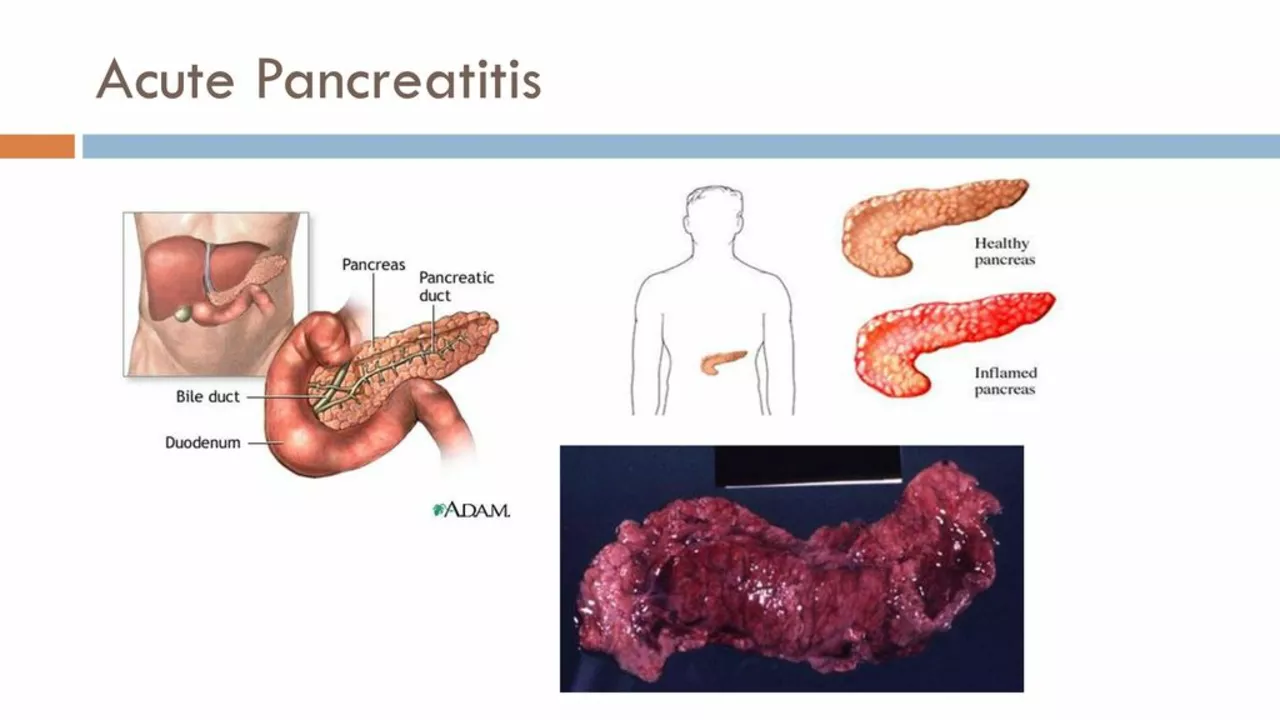
The pancreas sits behind your stomach and helps you digest food and control blood sugar. When it gets inflamed, that’s called pancreatitis. The swelling can be mild and go away on its own, or it can become severe and need urgent care.
Common causes you can avoid
The biggest culprits are heavy drinking and gallstones. Alcohol irritates the pancreas cells and makes them leak enzymes that start digesting the organ itself. Gallstones can block the tiny tube (duct) that carries these enzymes, causing a backup and inflammation.
Other triggers include certain medications like some antibiotics or steroids, high triglyceride levels, and rare infections. If you have any of these risk factors, keeping an eye on your diet and getting regular check‑ups can lower the odds of a flare‑up.
Symptoms that tell you something’s up
Sharp upper‑abdominal pain is the hallmark sign. The pain often radiates to the back and gets worse after eating, especially fatty meals. You might feel nauseous, vomit, or have a fever.
Some people notice rapid heartbeat, swollen abdomen, or oily stools that look greasy. If any of these appear suddenly, it’s time to call a doctor – pancreatitis can turn serious fast.
Doctors usually check blood tests for high enzyme levels (amylase and lipase) and order an ultrasound or CT scan to see the pancreas. These images help them decide if the inflammation is mild or needs more aggressive treatment.
Treatment options and home care
Mild cases often require fasting for a day or two, IV fluids, and pain relief. The goal is to let the pancreas rest while the body heals. Once you can tolerate food again, doctors suggest low‑fat meals and plenty of water.
Severe pancreatitis may need hospitalization, stronger pain meds, antibiotics if an infection is suspected, or even surgery to remove damaged tissue or gallstones.
After recovery, lifestyle changes make a big difference. Cut back on alcohol, keep your weight in check, eat balanced meals low in saturated fat, and manage blood sugar if you have diabetes. Regular follow‑up appointments let doctors monitor any long‑term damage.
If you’re looking for more detailed guides on specific meds or health topics, our site has articles about safe online pharmacy purchases, migraine alternatives, and many other drug‑related subjects that can help you stay informed.
The Connection between Pancreatic Duct Blockage and Autoimmune Diseases
In a recent study, I found a fascinating connection between pancreatic duct blockage and autoimmune diseases. The blockage in the pancreatic duct can lead to inflammation, which may trigger the immune system to attack the body's own tissues. This, in turn, can result in the development of autoimmune diseases like type 1 diabetes, celiac disease, and lupus. It's crucial to recognize these connections to find better treatment and prevention strategies for people suffering from these conditions. As a blogger, I am committed to raising awareness on this topic and promoting further research to improve the lives of those affected by autoimmune diseases.