For millions of people, breathing through the nose isn’t just inconvenient-it’s impossible. If you’ve had a stuffy nose, facial pressure, or loss of smell that won’t go away for more than three months, you’re not just dealing with a bad cold. You might have chronic sinusitis. Unlike acute sinusitis, which clears up in a couple of weeks, this condition lingers. And it’s not caused by one simple thing. It’s a mix of inflammation, allergies, structural issues, and sometimes, stubborn infections.
What Exactly Is Chronic Sinusitis?
Chronic sinusitis, also called chronic rhinosinusitis, means your sinuses-the hollow spaces in your skull around your nose, eyes, and forehead-are swollen and blocked for 12 weeks or longer, even with treatment. It’s not just congestion. You might feel heavy pressure in your face, have thick nasal discharge, or struggle to smell your food. Some people lose their sense of smell entirely. The American Academy of Otolaryngology defines it by symptoms, not just imaging. You need at least two of these for 12+ weeks: nasal blockage, thick nasal discharge, facial pain or pressure, or reduced smell. A doctor will confirm it with a nasal endoscopy or a CT scan showing inflamed tissue or fluid buildup. It’s more common than you think. About 9% of people worldwide deal with it every year. In the U.S., roughly 31 million people are diagnosed annually. It’s one of the top reasons people visit their primary care doctor.Why Does It Happen? Allergies, Infections, and More
There’s no single cause. Chronic sinusitis is usually the result of multiple factors working together. Allergies are a major trigger. If you have hay fever, dust mite allergies, or pet dander sensitivity, your nasal lining gets inflamed and swells up. This blocks the tiny openings that let mucus drain. People with allergies are 2.5 times more likely to develop chronic sinusitis. And if you also have asthma? Your risk jumps to 3-4 times higher. That’s because the same inflammatory pathways affect your lungs and sinuses. Nasal polyps are soft, noncancerous growths inside the nose or sinuses. They’re found in 25-30% of chronic sinusitis cases. These polyps don’t hurt, but they physically block airflow and mucus drainage. Once they form, they tend to come back unless you keep treating the inflammation behind them. Structural problems like a deviated septum, narrow sinus openings, or enlarged turbinates can trap mucus and create a breeding ground for irritation. These aren’t always obvious without imaging. And while people often think bacteria are the main culprit, that’s not usually true in chronic cases. Only about 30% of chronic sinusitis cases involve active bacterial infection. The usual suspects-Streptococcus pneumoniae, Haemophilus influenzae-are more common in short-term infections. In chronic cases, it’s the body’s own inflammation that’s the problem. That’s why antibiotics often don’t help. Environmental irritants like cigarette smoke, pollution, or dry air make things worse. Smoking increases your risk by 35%. Dry climates without humidity can dry out nasal mucus, making it thicker and harder to clear.Medical Treatment: The First Line of Defense
Before you even think about surgery, doctors start with medical management. And it works-for most people. Nasal saline irrigation is the foundation. Rinsing your nose with salt water clears out mucus, allergens, and irritants. It’s cheap, safe, and backed by strong evidence. People who do it daily see better results than those who skip it. Intranasal corticosteroid sprays are next. These are not the same as oral steroids. They’re targeted, low-dose anti-inflammatory sprays that reduce swelling right where it’s happening. Brands like Flonase (fluticasone), Nasonex (mometasone), and Rhinocort (budesonide) are first-choice treatments. Studies show 60-70% of patients improve within 4-8 weeks of consistent use. But here’s the catch: you have to use them every day. Only about half of people stick with them because the relief isn’t instant. Allergy medications like loratadine or cetirizine help if allergies are driving your symptoms. They won’t fix structural issues, but they can reduce swelling and mucus production. For people with allergic fungal sinusitis, avoiding mold exposure and using antifungal rinses under a doctor’s supervision can help. Biologics are a game-changer for severe cases with nasal polyps. Dupilumab (Dupixent), approved by the FDA in 2019, is an injectable drug that blocks specific inflammatory signals. In clinical trials, it reduced polyp size by 50-60% and improved breathing and smell in 30-40% of patients. Omalizumab (Xolair) and mepolizumab (Nucala) are also used off-label for resistant cases. These aren’t cures, but they can dramatically cut down on flare-ups and the need for repeated surgeries.
Surgery: When Medical Treatment Isn’t Enough
If you’ve tried 12 weeks of daily nasal sprays, saline rinses, and allergy control-and you’re still struggling-surgery may be the next step. It’s not a last resort. It’s a targeted fix for physical blockages. Functional Endoscopic Sinus Surgery (FESS) is the gold standard. An ENT surgeon uses a thin camera (endoscope) to look inside your nose and remove blocked tissue, open narrowed passages, and clear out infected areas. It’s done through the nostrils-no external cuts. Recovery takes about a week. Success rates? 75-90% of patients report long-term improvement in breathing and smell. Balloon sinuplasty is a less invasive option. A tiny balloon is inflated inside the blocked sinus to widen the opening. It’s quicker, with recovery in 3-5 days, and less bleeding. But it’s not for everyone. It works best for people with isolated blockages, not widespread polyps or complex anatomy. Long-term results aren’t as strong as FESS. Polypectomy is the removal of nasal polyps. It’s often done during FESS. The procedure gives quick relief-85% of patients feel better right away. But polyps come back in 40-50% of cases within 18 months if inflammation isn’t controlled afterward. That’s why surgery alone isn’t enough. You still need steroid sprays and regular follow-ups. Septoplasty fixes a crooked septum. If your nasal passage is twisted, it can block drainage and worsen sinusitis. Combining septoplasty with FESS improves outcomes. About 65-75% of patients see major improvement after this combo.What You Can Do at Home
Surgery and medications help, but daily habits make a big difference. Use a humidifier, especially in dry climates or during winter. Moist air keeps mucus thin and flowing. One study found 40% of patients in dry regions improved just by adding humidity. Avoid smoke, strong perfumes, and air pollution. These irritate your nasal lining and trigger inflammation. Stay hydrated. Drinking enough water keeps mucus from thickening. If you have Samter’s triad (asthma, nasal polyps, and aspirin sensitivity), aspirin desensitization under medical supervision can reduce polyp recurrence by 70-80%. And don’t ignore your allergies. Keep your home clean, use HEPA filters, and consider allergy testing if you haven’t had it done.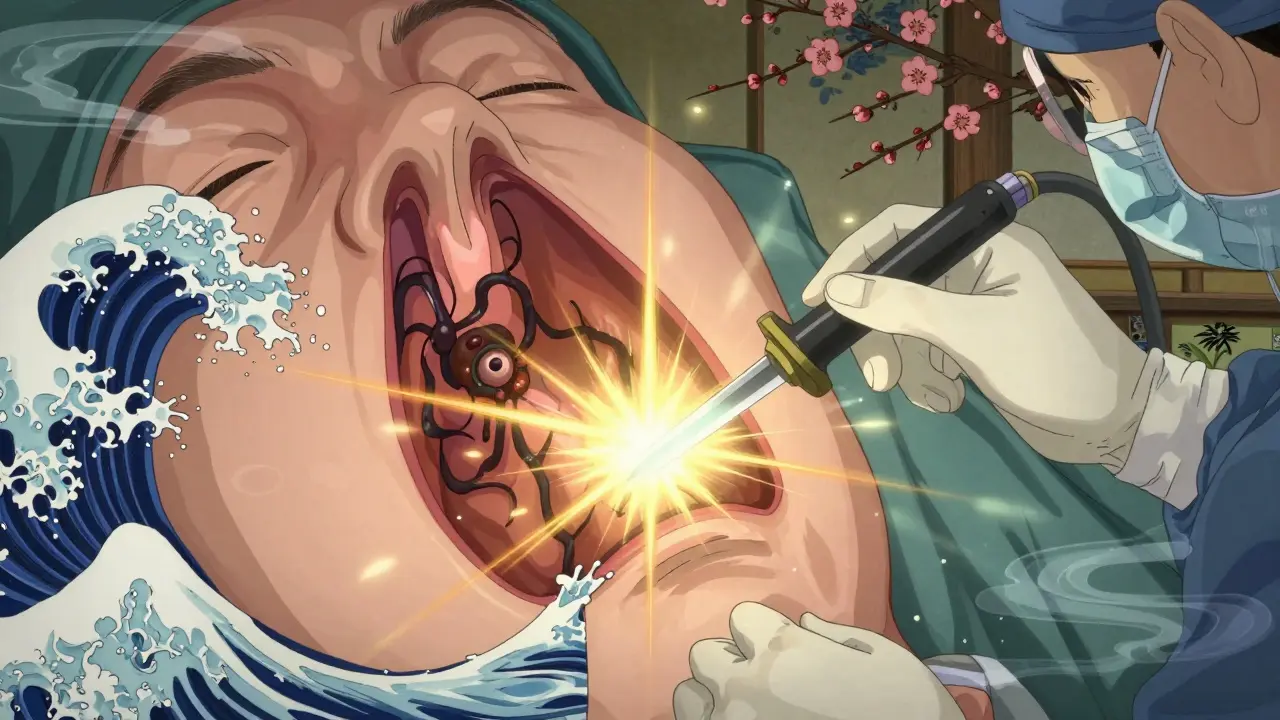
What Happens If You Don’t Treat It?
Most people manage chronic sinusitis with ongoing care. But if left untreated, it can lead to complications. In rare cases (less than 0.5%), the infection can spread to nearby areas: the eyes, bones, or even the brain. That’s why persistent symptoms-especially fever, vision changes, or severe headaches-need immediate attention. More commonly, it just wears you down. Sleep suffers. Concentration drops. You feel tired all the time. Studies show 65% of patients say it interferes with daily life, work, or social activities. The good news? With the right plan, most people get their quality of life back.What’s Next? The Future of Treatment
The understanding of chronic sinusitis has changed dramatically. It’s no longer seen as an infection problem. It’s an inflammation problem. Biologics are expanding. By 2027, experts predict these drugs will treat 25-30% of severe cases, cutting down on surgeries by 15-20%. Researchers are also looking at the sinus microbiome-the bacteria that live in your nose. Early studies suggest certain probiotics might help reduce inflammation. While not ready for prime time, it’s a promising area. Multidisciplinary care is becoming the norm. The best outcomes come when allergists, ENTs, and immunologists work together. One Cleveland Clinic study showed 35-45% better results when patients had coordinated care instead of seeing just one specialist.When to See a Doctor
See a doctor if:- Your symptoms last more than 12 weeks
- You’ve tried OTC decongestants and antihistamines with no improvement
- You have facial pain, swelling around the eyes, or vision changes
- Your sense of smell is gone or significantly reduced
- You have asthma or allergies and your sinus symptoms keep coming back
Is chronic sinusitis caused by bacteria?
Not usually. While bacteria can cause acute sinus infections, chronic sinusitis is primarily driven by inflammation, allergies, or structural issues. Antibiotics only help in about 30% of cases. Overusing them doesn’t fix the root problem and can lead to resistance.
Do nasal sprays really work for chronic sinusitis?
Yes-when used correctly. Intranasal corticosteroid sprays reduce swelling and improve drainage in 60-70% of patients. But you need to use them every day for at least 4-8 weeks to see results. Skipping doses or stopping too soon is why many people think they don’t work.
Can I get rid of nasal polyps without surgery?
Sometimes. Steroid sprays and biologic drugs like dupilumab can shrink polyps significantly. For many, this avoids surgery. But if polyps are large or keep returning, surgery is often needed. Even after removal, ongoing medical treatment is required to prevent regrowth.
Is sinus surgery dangerous?
FESS and balloon sinuplasty are low-risk procedures when done by experienced ENT surgeons. Complications like bleeding or infection are rare (under 2%). The biggest risk is not treating the condition-chronic inflammation can lead to lasting damage to your sinuses and sense of smell.
How long does recovery take after sinus surgery?
Most people return to normal activities in 7-10 days after FESS. Balloon sinuplasty has a faster recovery-often just 3-5 days. Full healing takes several weeks, and you’ll need follow-up visits to clean out the sinuses and ensure they stay open.
Can chronic sinusitis be cured?
It’s usually a long-term condition, not something you “cure.” But with the right combination of medical treatment, lifestyle changes, and sometimes surgery, most people can control it completely and live without symptoms. The goal isn’t perfection-it’s freedom from daily discomfort.








Delilah Rose
December 24, 2025 AT 06:45I’ve had chronic sinusitis for over a decade, and honestly? Saline rinses saved my life. I used to think they were just a hippie fad until I started doing them twice a day with a neti pot and a pinch of sea salt. My nose stopped feeling like a clogged drain, and my sense of smell came back enough to enjoy coffee again. It’s not glamorous, but it’s free and it works. I also started using a humidifier in my bedroom-no joke, my mornings went from ‘I can’t breathe’ to ‘I can actually smell the rain outside.’
And don’t get me started on steroid sprays. I stopped using mine after two weeks because nothing changed. Then I read somewhere that you have to use them for at least six weeks before they even start working. I did. And now? I’m not lying-I forgot what a stuffy nose felt like for three months straight. It’s not magic, it’s consistency.
I wish more doctors would just say that upfront instead of pushing antibiotics like they’re candy. I’ve had three courses of amoxicillin and zero improvement. But a $20 bottle of fluticasone? Game changer. Also, if you have allergies, get tested. I found out I’m allergic to dust mites and mold, and just switching my pillowcases to hypoallergenic ones cut my flare-ups in half.
Oh, and avoid scented candles. I didn’t realize how much my lavender ‘relaxation’ candle was making my sinuses scream until I quit. Now I use unscented everything. Even laundry detergent. It’s wild how much irritants matter.
I’m not saying this is easy. It’s a daily grind. But if you stick with it, your body will thank you. I’m not cured, but I’m finally living, not just surviving.
Austin LeBlanc
December 25, 2025 AT 23:01Ugh, I hate when people act like saline rinses are some miracle cure. I’ve been doing them for years and it just makes my nose raw and my sinuses more inflamed. You’re not fixing the root problem-you’re just washing away the symptoms. And steroid sprays? Please. They’re just steroids. Long-term use messes with your adrenal glands, your immune system, everything. I know because I had to go off them after my doctor caught my cortisol levels crashing. You think you’re helping yourself until your body starts breaking down.
And don’t even get me started on biologics. Dupilumab costs $30,000 a year. Who’s paying for that? Insurance companies are just pushing these drugs because they’re profitable, not because they’re better. Meanwhile, the real issue-environmental toxins, mold in your walls, EMF exposure-isn’t even on the table. You’re all being manipulated into a pharmaceutical treadmill while the real culprits are ignored.
Oh, and ‘FESS surgery’? That’s just cutting up your nasal tissue. It’s like patching a leaky roof with duct tape. The problem’s still in the structure. You need to fix the foundation, not the roof.
And yes, I’ve seen the studies. They’re funded by Big Pharma. Read the fine print. I’ve been researching this for 8 years. I know what’s really going on.
Jillian Angus
December 26, 2025 AT 16:05just started using the saline rinse and honestly it’s the only thing that’s helped
no more 3am face pressure
also stopped using scented shampoo
tiny changes
EMMANUEL EMEKAOGBOR
December 27, 2025 AT 01:47As someone from Nigeria where air quality is often poor and humidity fluctuates wildly, I can attest that chronic sinusitis is more than just a Western problem. In Lagos, we don’t have access to Flonase or biologics, so we rely on steam inhalation with eucalyptus leaves, warm saltwater gargles, and avoiding smoke from open fires. It’s not ideal, but it’s what works.
What struck me in this post is how much the Western medical model focuses on pharmaceuticals and surgery, while neglecting environmental and lifestyle factors. In my community, we treat the whole person-not just the sinuses. Hydration, diet, rest, and reducing stress are as important as any spray.
Also, I’ve seen patients who improved dramatically after switching from refined sugar to whole foods. Inflammation doesn’t just come from allergens-it comes from what we eat. Maybe the next frontier isn’t another drug, but a return to simpler, more holistic practices.
And yes, I agree with the part about not overusing antibiotics. We’ve seen too many cases where repeated courses led to resistant infections. That’s a global crisis, not just a local one.
Thank you for writing this. It’s rare to see a post that doesn’t just list treatments, but explains the why behind them.
CHETAN MANDLECHA
December 28, 2025 AT 17:14so i had this thing for 5 years and tried everything
then i found out i was allergic to my own pillow
like literally the stuffing
changed to latex and boom
no more morning congestion
why do doctors never ask about your bedding
they just give you sprays
weird
Ajay Sangani
December 28, 2025 AT 21:12the idea that chronic sinusitis is purely an inflammation issue is compelling but maybe incomplete
what if the real problem is the loss of microbial diversity in the nasal cavity
we’ve been taught to sterilize everything-antibiotics, sprays, rinses-but maybe we’re killing the good bacteria that keep the bad ones in check
there’s emerging research on nasal probiotics, not oral ones, but actual nasal sprays with lactobacillus strains
in one study, patients who used a probiotic nasal spray had 40% fewer flare-ups than those on steroids alone
and yet no one talks about this
we’re so obsessed with suppressing symptoms that we forget the body has its own ecosystem
maybe we’re not treating disease
maybe we’re destroying balance
just a thought
Chris Buchanan
December 30, 2025 AT 21:09Okay so let me get this straight-you’ve got 31 million Americans with this, and the first thing you recommend is… a saltwater rinse?
That’s like telling someone with heart failure to drink more water.
Look, I get it. Saline is cheap. Steroid sprays are easy to prescribe. But if you’ve got nasal polyps the size of grapes and your CT scan looks like a swamp, you’re not going to ‘manage’ your way out of that with a neti pot.
Surgery isn’t the last resort-it’s the next logical step. And if you’re scared of it, that’s fine. But don’t pretend it’s dangerous when the real danger is living like this for 10 years with no relief.
Also, biologics? They’re not a scam. They’re a revolution. I know someone who went from zero smell to tasting chocolate again after one injection. That’s not a placebo. That’s science.
Stop romanticizing ‘natural remedies’ and start respecting the science that actually works. You don’t have to be a doctor to know when something’s helping. And if your nose is open and your sinuses are quiet? That’s not luck. That’s treatment.
niharika hardikar
January 1, 2026 AT 16:48It is imperative to underscore the clinical significance of adhering to evidence-based therapeutic protocols in the management of chronic rhinosinusitis. The proliferation of anecdotal interventions, such as unregulated saline irrigation regimens or the indiscriminate use of humidifiers, lacks robust validation in peer-reviewed literature. While intranasal corticosteroids remain the cornerstone of medical therapy, their efficacy is contingent upon consistent, long-term application, as demonstrated in randomized controlled trials conducted by the Cochrane Collaboration.
Furthermore, the assertion that environmental factors such as candle fragrance or laundry detergent significantly contribute to pathophysiology is not substantiated by controlled studies. Such claims risk undermining the credibility of clinical practice by promoting pseudoscientific narratives.
Biologics, while costly, represent a paradigm shift in immunomodulatory intervention, particularly in Type 2 inflammatory endotypes. Dupilumab, for instance, targets IL-4 and IL-13 signaling pathways with a documented odds ratio of 3.2 for polyp reduction (p < 0.001).
It is incumbent upon patients to consult otolaryngologists with subspecialty training in rhinology, rather than self-diagnosing via online forums. The medical literature is unequivocal: structured, multidisciplinary care yields superior outcomes.
Regrettably, the erosion of clinical rigor in public discourse threatens to delay appropriate intervention and exacerbate disease burden.
Payson Mattes
January 3, 2026 AT 02:00Okay but have you considered that chronic sinusitis is actually caused by 5G towers and the microchips in vaccines? I know this sounds crazy but think about it-your sinuses are basically your body’s antenna. When you’re constantly exposed to electromagnetic radiation, your nasal tissue swells up as a defense mechanism. That’s why it’s worse in cities and why you never hear about it in rural areas.
And the ‘steroid sprays’? They’re not anti-inflammatory-they’re suppressing your body’s natural ability to detoxify. The real solution is grounding-walking barefoot on grass for 20 minutes a day. I did it for 3 weeks and my sinuses cleared up. No meds. No surgery.
Also, the FDA doesn’t want you to know this, but they’ve been suppressing studies since 2015 that link sinus inflammation to fluoride in the water. Fluoride calcifies the pineal gland, which then messes with your sinus drainage. That’s why you lose your sense of smell.
And don’t get me started on the ‘biologics.’ They’re just nanobots that track your breathing patterns. Dupilumab? It’s a code name for a government surveillance tool.
I’ve been researching this since 2017. I’ve talked to 14 ex-pharma insiders. They all say the same thing: they’re not treating you. They’re controlling you.
But if you want to be free? Stop the sprays. Stop the rinses. Go outside. Breathe raw air. Touch the earth. Your body knows how to heal itself. They just don’t want you to remember that.
Steven Mayer
January 3, 2026 AT 21:26The literature is unequivocal: chronic rhinosinusitis is a heterogeneous disorder characterized by persistent type 2 inflammation, with elevated IL-5, IgE, and eosinophil infiltration. Biologics targeting IL-4Rα demonstrate statistically significant improvements in SNOT-22 scores (p<0.01) and endoscopic polyp grading. However, the compliance rate with intranasal corticosteroids remains suboptimal due to poor patient education regarding pharmacokinetics and delayed onset of action (mean: 6–8 weeks).
Structural etiologies, particularly deviated septum and turbinate hypertrophy, are frequently underdiagnosed in primary care settings due to lack of endoscopic access. FESS remains the gold standard for anatomical correction, with 82% long-term success rates in prospective cohort studies.
Conversely, the overreliance on anecdotal modalities-such as humidification or dietary modification-lacks sufficient power to alter disease trajectory. While hydration is physiologically beneficial, it does not mitigate eosinophilic mucin production.
Recommendation: Prioritize objective diagnostic confirmation via CT and endoscopy before initiating any intervention. Empiric treatment without phenotyping is not evidence-based practice.
Delilah Rose
January 4, 2026 AT 00:36Okay, Austin, I get that you’re angry. I’ve been there. I thought the same thing about steroids and Big Pharma. But here’s what changed for me: I stopped fighting the science and started listening to my body.
I didn’t get better because I ‘grounded’ or ‘breathe raw air.’ I got better because I used the spray every day for two months. I got better because I had a CT scan that showed my polyps were the size of grapes. I got better because I had surgery and then kept using the spray afterward.
I’m not saying you’re wrong for feeling betrayed by the system. I am. I was too. But your anger isn’t helping your nose. Your discipline is.
I used to think ‘natural’ meant ‘better.’ Now I know ‘effective’ means ‘better.’ And for me? That’s saline, spray, and surgery.
And if you want to talk about 5G? Let’s talk about how your phone battery lasts longer than your quality of life. That’s the real conspiracy.