Fertility Preservation Options Guide
Fertility Preservation Options Guide
What Are Your Options?
Facing a rhabdomyosarcoma diagnosis is scary enough, but worries about future family plans can add another layer of stress. This guide breaks down what the disease and its treatment mean for your reproductive health and shows you concrete steps to protect fertility before, during, and after therapy.
What Is Rhabdomyosarcoma?
Rhabdomyosarcoma is a rare, fast‑growing soft‑tissue cancer that arises from skeletal‑muscle precursors. It most often appears in children and teens, accounting for about 3‑4% of all pediatric cancers. The disease is classified mainly into two subtypes: embryonal (more common in younger kids) and alveolar (tends to affect older adolescents).
According to the International Society of Pediatric Oncology, roughly 350 new cases are diagnosed in the United States each year, and survival rates have risen to 70‑80% thanks to multimodal treatment.
How Standard Treatments Impact Fertility
Modern rhabdomyosarcoma protocols combine surgery, chemotherapy, and radiation therapy. Each component carries its own risk to the reproductive system.
- Chemotherapy uses drugs like cyclophosphamide and ifosfamide that can damage ovarian follicles in women and spermatogenic cells in men. The dose and duration dictate the severity.
- Radiation therapy directed at the pelvis or abdomen can permanently scar the uterus, ovaries, or testes, markedly reducing the chance of natural conception.
- Surgical removal of tumors located near reproductive organs may require partial or total organ excision, which obviously eliminates the natural function of the removed tissue.
Understanding Rhabdomyosarcoma fertility concerns is the first step toward proactive planning.
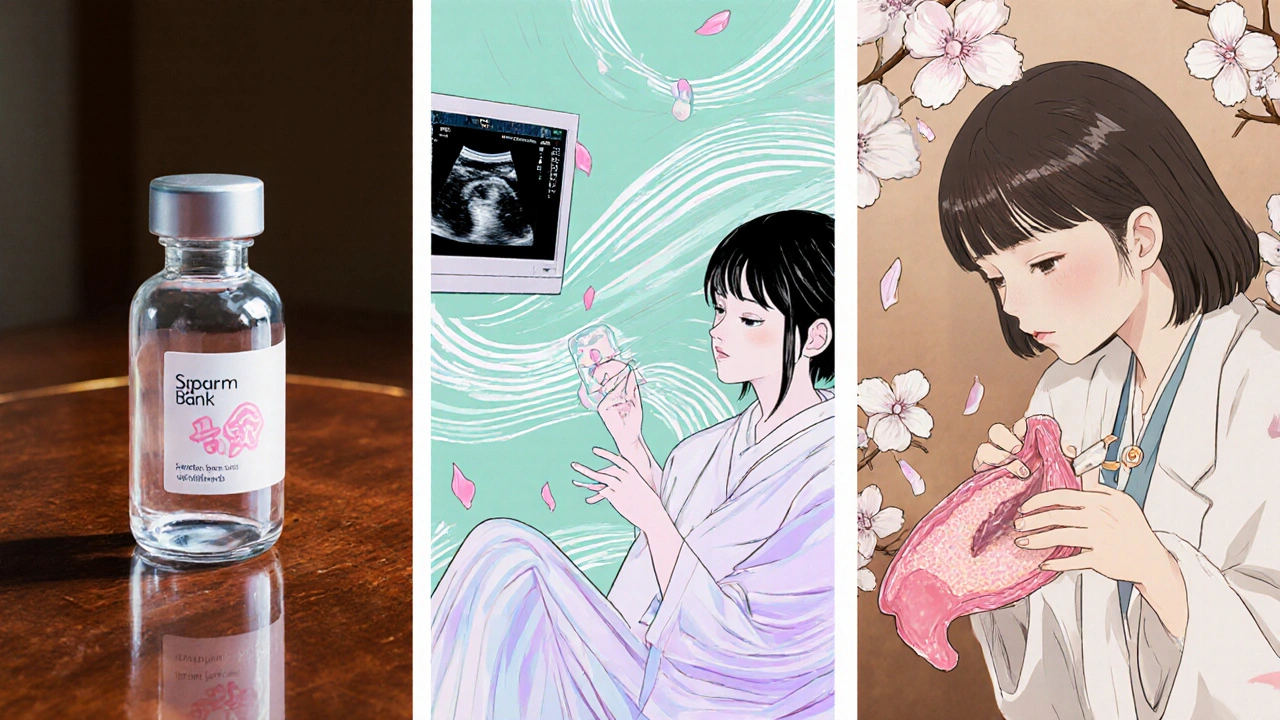
Fertility Preservation Options
Fortunately, a range of techniques exists to safeguard future parenthood. The right choice depends on age, gender, disease stage, and timing of treatment.
| Method | Success Rate (Live Birth) | Typical Age Range | Procedure Time | Key Pros | Key Cons |
|---|---|---|---|---|---|
| Sperm Banking | ≈70‑80% | Adolescents ≥ 12 y | 1‑2 weeks | Non‑invasive, quick | Requires mature sperm, storage cost |
| Egg Freezing (Vitrification) | ≈50‑60% | Females ≥ 13 y | 2‑3 weeks (stimulation) | High survival of eggs | Hormonal stimulation, cost |
| Ovarian Tissue Banking | ≈30‑40% (experimental) | All ages, incl. pre‑pubertal | 1‑2 days (surgery) | Option for young girls | Experimental, re‑implantation risks |
| Testicular Tissue Preservation | Experimental | Pre‑pubertal boys | 1‑2 days (surgery) | Only option before puberty | Still in research, no live births yet |
| Gonadal Shielding (Radiation) | Preserves existing function | Applicable to both sexes | Integrated with RT plan | Non‑invasive | Only reduces, doesn’t eliminate risk |
Each method has its own set of eligibility criteria. Younger patients who haven’t yet entered puberty can’t produce eggs or sperm, so tissue banking becomes the primary route. Older teens and adults often opt for sperm banking or egg freezing, which have higher success rates and are widely available.
Making the Decision: Questions to Ask Your Care Team
- Will my treatment field include the pelvis or abdomen? If so, can gonadal shielding be used?
- What chemotherapy agents and cumulative doses are planned? Some drugs are more gonadotoxic than others.
- How much time do I have before treatment starts? Egg or sperm banking usually needs a 1‑2‑week window.
- Do I qualify for experimental tissue banking programs? Many academic centers run trials.
- What are the costs and insurance coverage for each option? Factor in long‑term storage fees.
Write down the answers and bring a trusted family member to the appointment. Having a clear record helps you compare options later.
After Treatment: Monitoring and Restoring Fertility
Once therapy is complete, your doctor will schedule follow‑up labs to assess hormonal levels.
- For women, measuring FSH and AMH can indicate ovarian reserve.
- For men, a semen analysis at 6‑12 months post‑chemo shows whether spermatogenesis has recovered.
If natural fertility is compromised, assisted reproductive technologies (ART) such as IVF + ICSI can use previously banked gametes. Hormone replacement therapy may also be an option to protect bone health while waiting for potential recovery.

Emotional Support and Practical Resources
Fertility worries sit alongside the usual fear of cancer. Connecting with peers who have walked the same path can ease anxiety.
- National organizations like the American Childhood Cancer offer fertility‑specific counseling.
- Online forums (e.g., #RhabdoFertility on social media) let you share experiences and tips.
- Hospital social workers often coordinate financial assistance for storage fees.
Don’t hesitate to ask for a referral to a reproductive endocrinologist or a male fertility specialist. Early involvement improves the odds of retaining options.
Key Takeaways
- Rhabdomyosarcoma treatments can damage sperm, eggs, and reproductive organs, but many preservation methods exist.
- Sperm banking and egg freezing have the highest success rates; ovarian or testicular tissue banking are options for pre‑pubertal patients.
- Ask your oncology team about gonadal shielding, drug‑specific risks, and timing to fit preservation into your treatment schedule.
- Post‑treatment hormone monitoring tells you whether natural conception is still possible or if ART is needed.
- Emotional support resources are vital-connect with survivorship groups, counseling services, and financial aid programs early.
Can I still have children after chemotherapy for rhabdomyosarcoma?
Many patients regain partial or full fertility after chemotherapy, especially if lower‑dose regimens were used. However, the likelihood varies by age, drug type, and cumulative dose. Banking sperm or eggs before treatment provides a safety net.
Is ovarian tissue banking safe for a 10‑year‑old girl?
Ovarian tissue banking is considered experimental but has been performed safely in children. The tissue is frozen shortly after removal and can be re‑implanted later. Success rates are still improving, but it remains the only option for pre‑pubertal girls.
How much does sperm or egg banking cost in Australia?
In Sydney, sperm banking typically costs AU$150-200 for the initial collection plus AU$100-150 per year for storage. Egg freezing starts around AU$7,000-9,000 for the cycle, with annual storage fees of AU$500-800. Some private health funds and charities offer partial rebates.
What is gonadal shielding and can it replace sperm banking?
Gonadal shielding uses lead blocks during radiation therapy to reduce dose to the testes or ovaries. It helps preserve existing cells but does not guarantee fertility, especially when chemotherapy is also used. It’s best used alongside a banking strategy.
When should I schedule follow‑up fertility testing?
For women, hormone panels are usually drawn 6‑12 months after completing chemo. Men should have a semen analysis at 6 months, with repeat testing if results are poor. Your oncologist can coordinate these appointments.








Rakhi Kasana
October 19, 2025 AT 15:11Many families focus on beating the tumor first, but they often postpone the fertility conversation until after surgery. That delay can lock out options like ovarian tissue banking that need to happen before chemo begins. Even a brief chat with a reproductive specialist can map out a timeline that fits the oncology schedule.
Sarah Unrath
October 29, 2025 AT 02:11i think u should ask ur doc bout sperm banking asap
James Dean
November 7, 2025 AT 14:11It’s worth remembering that the gonadotoxic impact of cyclophosphamide is dose‑dependent so a lower cumulative exposure may still leave some spermatogenic reserve you can test later with a semen analysis.
Monika Bozkurt
November 17, 2025 AT 02:11The interdisciplinary management of rhabdomyosarcoma necessitates a synchronized integration of oncologic control and onco‑fertility preservation strategies.
Recent consensus guidelines underscore the importance of pre‑treatment counseling to delineate individualized risk stratification based on chemotherapeutic agents, radiation fields, and patient age.
Cyclophosphamide and ifosfamide, classified as alkylating agents, exhibit a dose‑response relationship with ovarian follicular depletion, quantified by anti‑Müllerian hormone (AMH) trajectories.
In male patients, the same agents induce DNA cross‑linking in spermatogonia, leading to transient azoospermia that may resolve after a latency period contingent upon the cumulative dose.
Radiation therapy directed at the pelvis precipitates irreversible compromise of gonadal stromal architecture, a phenomenon that gonadal shielding can partially mitigate but not fully obviate.
Sperm cryopreservation remains the gold standard for post‑pubertal males, achieving live‑birth rates approximating 70‑80 % per thawed sample in contemporary series.
For females, controlled ovarian stimulation followed by vitrification yields a comparable success metric, albeit tempered by the need for adequate ovarian reserve and the risk of hormone‑sensitive tumor progression.
Ovarian tissue cryopreservation extends feasibility to pre‑pubertal girls, though re‑implantation carries a theoretical risk of malignant cell reintroduction, warranting rigorous histopathologic screening.
Emerging in‑vitro follicle maturation techniques hold promise to circumvent re‑implantation concerns, yet remain investigational.
Financial considerations are non‑trivial; insurance coverage varies widely across jurisdictions, and out‑of‑pocket expenses for storage can accumulate over decades.
Multidisciplinary fertility preservation programs often incorporate social work liaisons to navigate grant opportunities and philanthropic assistance.
Post‑treatment surveillance should include serial AMH and FSH measurements for females and semen analyses at six‑month intervals for males to objectively gauge gonadal recovery.
Should endogenous function remain insufficient, assisted reproductive technologies such as intracytoplasmic sperm injection (ICSI) or pre‑implantation genetic testing (PGT‑M) can be employed using the previously cryopreserved gametes.
Psychosocial support remains a cornerstone, as fertility concerns frequently intersect with identity, body image, and future family planning aspirations.
In sum, proactive, informed decision‑making, anchored in evidence‑based risk assessment, optimizes the likelihood of preserving reproductive potential without compromising oncologic outcomes.
Ben Bathgate
November 26, 2025 AT 14:11Sounds solid, but honestly the cost of egg freezing can be a nightmare for most families, and not every clinic even offers the latest vitrification protocols.
Bobby Marie
December 6, 2025 AT 02:11The key is to get the referral early; waiting even a few weeks can cut out viable options.
Christian Georg
December 15, 2025 AT 14:11When you’re gearing up for preservation, start by asking your oncologist for a referral to a reproductive endocrinologist - they’ll run baseline hormone panels, discuss stimulation protocols, and coordinate timing so you don’t miss the prep window 😊. Make sure you confirm insurance benefits early; many plans cover at least one year of storage, and you can often apply for charity assistance through cancer foundations. Also, keep a written log of medication dosages and dates; it’s vital for your future fertility specialist to understand the total gonadotoxic exposure.
Christopher Burczyk
December 25, 2025 AT 02:11In addition to the steps outlined, it is advisable to secure a detailed written treatment summary from the oncology team, including cumulative cyclophosphamide equivalents, to facilitate precise prognostication of ovarian reserve loss.
Caroline Keller
January 3, 2026 AT 14:11Your future kids deserve you to fight for every option!
Maridel Frey
January 13, 2026 AT 02:11Building a support network that includes oncologists, fertility specialists, and peer mentors can substantially alleviate the emotional burden associated with navigating these complex decisions.
Madhav Dasari
January 22, 2026 AT 14:11Totally agree-having a squad of people who’ve been through the same hoopla makes the whole process feel less like a solo mission and more like a team sport.
Jameson The Owl
February 1, 2026 AT 02:11The pharma industry has a vested interest in keeping fertility preservation under‑advertised because it limits the market for their costly fertility drugs. By downplaying the risks, they ensure patients focus solely on survival, not on future parenthood. Moreover, insurance companies are often coaxed into offering minimal coverage, forcing families to foot the bill for cryopreservation. Independent studies have repeatedly shown that early intervention improves outcomes, yet these findings are buried in pay‑walled journals. Patients should demand transparency and push for legislative mandates that require oncologists to discuss fertility as a standard of care.
Catherine Viola
February 10, 2026 AT 14:11It is imperative, therefore, to integrate a multidisciplinary onco‑fertility protocol at the point of diagnosis, encompassing cytotoxic exposure quantification, gonadal shielding feasibility assessments, and expedited gamete preservation pathways to safeguard reproductive autonomy.
sravya rudraraju
February 20, 2026 AT 02:11Embarking on the journey of cancer treatment while contemplating future parenthood can feel like walking a tightrope stretched over a chasm of uncertainty. Yet, the convergence of modern oncologic regimens and advanced reproductive technologies offers a beacon of hope that should not be dismissed. By proactively engaging with a dedicated fertility preservation team, patients can map out individualized strategies that align with their therapeutic timeline. The selection of appropriate modalities-whether sperm banking, oocyte vitrification, or ovarian tissue cryopreservation-must be guided by age, disease stage, and personal aspirations. Importantly, early hormonal profiling, including AMH and FSH levels, provides critical data to forecast ovarian reserve decline. Financial planning, too, is a cornerstone; exploring institutional grants, charitable foundations, and potential employer benefits can mitigate the economic strain. Emotional resilience is fortified through peer support groups, wherein shared experiences demystify the process and normalize the associated anxieties. Ultimately, a holistic approach that synergizes medical, psychological, and logistical dimensions empowers patients to preserve the possibility of building families in the aftermath of remission.