Every year, hundreds of thousands of people in the U.S. are hurt by medication mistakes made right in their own homes. These aren’t rare accidents-they happen more often than you think. A child gets the wrong dose of Tylenol because the bottle looked similar to another. An elderly parent misses a dose because the pill organizer wasn’t labeled clearly. Someone takes an old prescription they forgot was discontinued. These aren’t just mistakes-they’re preventable dangers.
What Are the Most Common Medication Errors at Home?
The biggest problems aren’t always about taking too much. Often, it’s about taking the wrong thing, at the wrong time, or not taking it at all. According to data from the Agency for Healthcare Research and Quality, the top three errors in home settings are: giving the wrong dose, missing doses, and giving the wrong medication entirely.
For kids, confusion between infant and children’s strengths of acetaminophen or ibuprofen is a major issue. Infant Tylenol is more concentrated. If a parent uses the dropper from the children’s bottle by accident, they could give a dose that’s too high-sometimes dangerously so. A 2023 study from UC Davis Health found that nearly half of parents mix up these formulations.
For older adults, the problem grows with the number of pills. People taking five or more medications daily have a 30% higher chance of making a mistake. Those over 75? The risk jumps to 38%. It’s not just forgetting. It’s mixing up names, confusing brand and generic versions, or taking something because it “looks familiar.”
Another silent killer? Stopping antibiotics early. Studies show that 92.7% of parents prescribed antibiotics for ear infections gave fewer doses than required. That doesn’t just make the infection worse-it helps create drug-resistant bacteria.
Why Do These Mistakes Keep Happening?
It’s not because people are careless. It’s because the system isn’t designed for clarity.
Most people leave the doctor’s office with too much information and not enough understanding. Research shows that 40% to 80% of what patients hear during a medical visit is forgotten or misunderstood by the time they get home. That’s not a failure of memory-it’s a failure of communication.
Confusing labels make it worse. Look-alike, sound-alike drug names like Hydralazine and Hydroxyzine are easy to mix up. Even the bottle design can trick you. Some medications come in similar-colored bottles with nearly identical caps. One wrong twist, and you’ve given your child the wrong medicine.
Cost is another hidden factor. People skip doses because they can’t afford the full prescription. Others take extra pills because they’re desperate to feel better. Neither is safe, but both are common.
And then there’s the clutter. Pill organizers with no labels. Medicine cabinets full of expired drugs. Notes scribbled on napkins about “take 2 after lunch.” It’s no wonder mistakes happen.
How to Prevent Wrong Doses and Mix-Ups
Preventing errors doesn’t require a PhD. It just needs simple, consistent habits.
- Always check the label for weight and age-not just volume. A teaspoon isn’t always a teaspoon. Use the measuring tool that came with the medicine. Never use a kitchen spoon.
- Never alternate acetaminophen and ibuprofen unless a doctor specifically tells you to. Doing so increases the chance of error by 47%, according to pediatric research. Stick to one unless instructed otherwise.
- Keep a live medication list. Write down every pill, liquid, patch, or injection you or your loved one takes-including vitamins and over-the-counter drugs. Update it every time something changes. Share this list with every doctor, pharmacist, and caregiver.
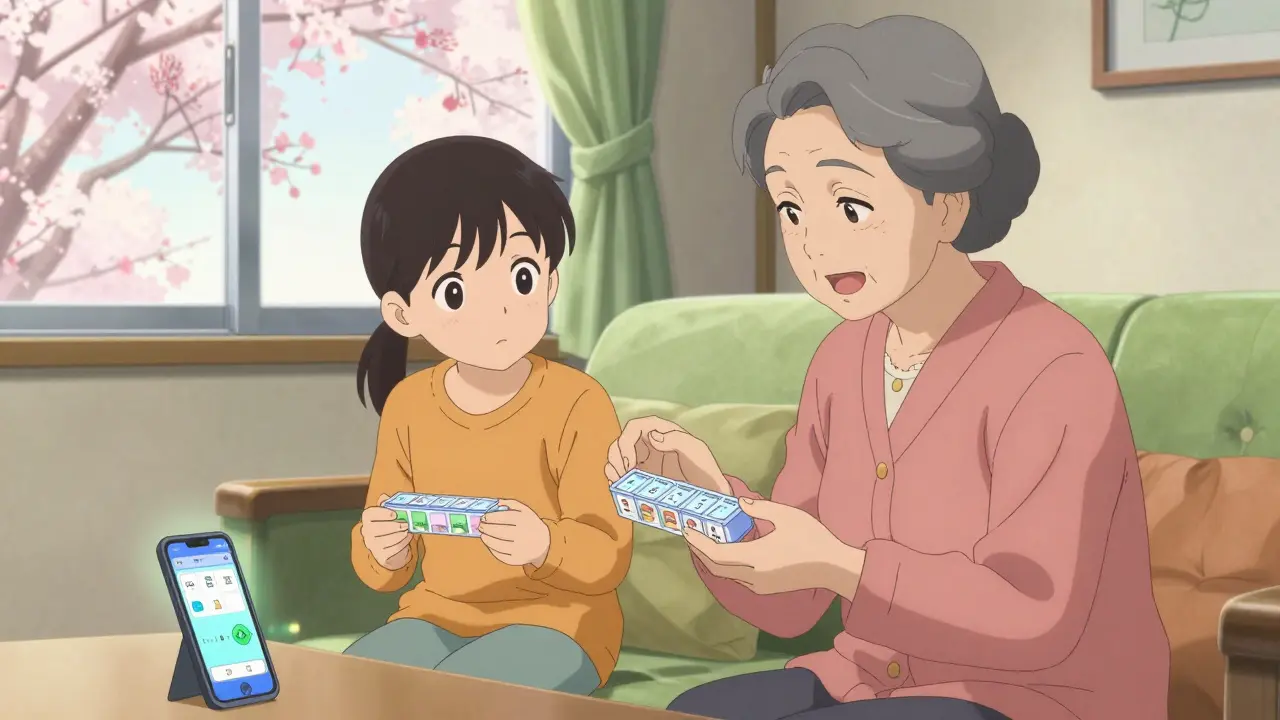
- Use a pill organizer with clear labels. Buy one with large print and separate compartments for morning, afternoon, evening, and night. Write the drug name and dose directly on each section with a permanent marker.
- Ask for one concentration. If your child needs regular doses of Tylenol or ibuprofen, ask your doctor if they can prescribe the same strength for both infant and child versions. That eliminates one major point of confusion.

Don’t Let Old Medications Lurk in the Cabinet
Expired or unused drugs are ticking time bombs. People keep them “just in case.” But that “just in case” can become a deadly mistake.
Studies show that nearly 27% of nursing home medication errors trace back to discharge instructions that weren’t properly followed at home. That includes taking drugs that were stopped at the hospital. One man took his old blood pressure pill after being discharged-only to find out his doctor had switched him to a new one. He ended up in the ER with dangerously low blood pressure.
Here’s what to do:
- When you get home from the hospital, sit down with your list and cross out anything your doctor said to stop.
- Check expiration dates every six months. If it’s old, blurry, or smells weird, throw it out.
- Don’t flush pills down the toilet. Take them to a pharmacy drop-off or local drug take-back event. Many pharmacies now offer free disposal.
Use the Teach-Back Method to Make Sure You Understand
Doctors don’t always know how confusing their instructions sound. That’s why the “teach-back” method works so well.
After your doctor or pharmacist explains how to take a new medicine, say: “Can you please check if I got this right?” Then explain it back in your own words. “So, I take one of these pills every morning with food, not at night, and I stop after seven days, even if I feel better?”
This simple step cuts errors by nearly half. It’s not about testing you-it’s about making sure the message was heard correctly. The Agency for Healthcare Research and Quality recommends this for every new prescription.
Ask the Right Questions Before You Leave the Clinic
Don’t wait until you’re home to realize you’re confused. Ask these five questions before you walk out the door:
- What is this medicine for?
- How and when do I take it? (With food? At bedtime? Every 8 hours?)
- How long should I take it?
- What side effects should I watch for?
- What should I do if I miss a dose?
If the answer is vague-“take as needed” or “follow the label”-ask for specifics. “What does ‘as needed’ mean? Can I take it three times a day or just once?”
When You’re Caring for Someone Else
If you’re helping a parent, partner, or child with their meds, you’re part of the safety team.
Here’s what works:
- Don’t assume they remember the instructions. Even if they’re sharp, stress and aging can cloud memory.
- Set phone alarms for doses. Label them clearly: “Morning Blood Pressure Pill” or “Evening Antibiotic.”
- Use a digital app like Medisafe or MyTherapy to track doses. Many send reminders and let you log who gave the pill.
- Have a backup plan. If you’re away for the weekend, make sure someone else knows the schedule and has access to the meds.
Final Thought: Safety Is a Habit, Not a One-Time Fix
Medication safety isn’t about being perfect. It’s about building routines that reduce risk. One mistake can lead to a hospital visit. Two mistakes can lead to lasting harm. But with a few clear steps-checking labels, keeping lists, asking questions-you can protect yourself and your family.
Start today. Grab that medicine cabinet. Clear out the old pills. Write down the current list. Set a reminder to check it again in two weeks. That’s how real safety begins-not with a grand plan, but with one small, smart action.








Ted Conerly
January 10, 2026 AT 21:48One thing no one talks about is how pharmacies still print labels in 6-point font. I had to use a magnifying glass last week to read my mom’s blood pressure med instructions. If you’re over 70, you’re basically being punished for aging. Use the app that lets you scan the barcode and get a voice reading. It’s free. Do it.
McCarthy Halverson
January 11, 2026 AT 14:51Use the original container. Never transfer pills. Even if the organizer looks neat. The bottle has the barcode, expiration, and lot number. That’s not optional.
Mario Bros
January 11, 2026 AT 17:31My grandma used to keep all her meds in a cereal box because ‘it was easier to find’. I laughed until I realized she’d been taking her insulin out of a Lucky Charms box for 3 years. 😅 Get a real organizer. Seriously.
Jake Nunez
January 13, 2026 AT 06:06In my community, a lot of folks skip doses because they’re afraid of side effects or don’t trust doctors. We need more bilingual pharmacists and home visits-not just pamphlets in English. Language isn’t just about translation. It’s about trust.
Christine Milne
January 13, 2026 AT 17:32This article is dangerously naive. The real problem is that pharmaceutical companies design drugs to be confusing. Look-alike packaging, sound-alike names-this isn’t negligence, it’s corporate strategy. And now we’re supposed to blame grandparents for not memorizing 17 pills a day? The system is broken, not the patients.
Dwayne Dickson
January 14, 2026 AT 01:37While the practical advice herein is commendable, one must not overlook the structural determinants of pharmaceutical mismanagement. The conflation of pharmacokinetic principles with layperson comprehension is a pedagogical failure of systemic proportion. The reliance upon mnemonic devices and pill organizers presupposes a baseline of executive function that is neither equitably distributed nor adequately supported by public health infrastructure. Moreover, the normalization of ‘teach-back’ methodology, though empirically validated, remains underutilized due to time constraints imposed by fee-for-service reimbursement models-a perverse incentive structure that prioritizes throughput over safety. Until regulatory agencies mandate standardized labeling protocols and prohibit the co-packaging of high-risk medications with indistinguishable visual profiles, we are merely rearranging deck chairs on the Titanic.
Michael Marchio
January 15, 2026 AT 01:58You people are missing the point entirely. This isn’t about labels or apps or teach-backs. It’s about people being lazy. If you can’t remember to take your medicine, maybe you shouldn’t be in charge of it. My uncle took his wife’s thyroid med by accident because he didn’t bother to read the bottle-twice. He ended up in the hospital. He was 68. He had a PhD. He watched TV for 10 hours a day. The problem isn’t the system. It’s the people who refuse to take responsibility. If you’re too busy or too tired to manage your meds, get someone to help you. Or don’t take them. But don’t act like it’s the pharmacist’s fault when you mix up Clonazepam and Clonidine because you were too distracted to look.
Bradford Beardall
January 15, 2026 AT 16:08Has anyone here tried the new FDA-approved pill identifiers that use QR codes? Scan it and it tells you the drug, dose, purpose, and expiry in plain language. My local CVS just started rolling them out. Took me 5 seconds to scan my dad’s meds and realize he’d been taking the wrong statin for 6 months. No joke. The system’s broken, but tech is catching up. Let’s not ignore the solutions that already exist.