Pancreatic Cancer Risk Calculator
Personal Risk Factors
Your Pancreatic Cancer Risk
0%
Your risk is similar to average
Based on the latest scientific evidence, your calculated risk shows how your lifestyle factors compare to the general population.
Personalized Recommendations
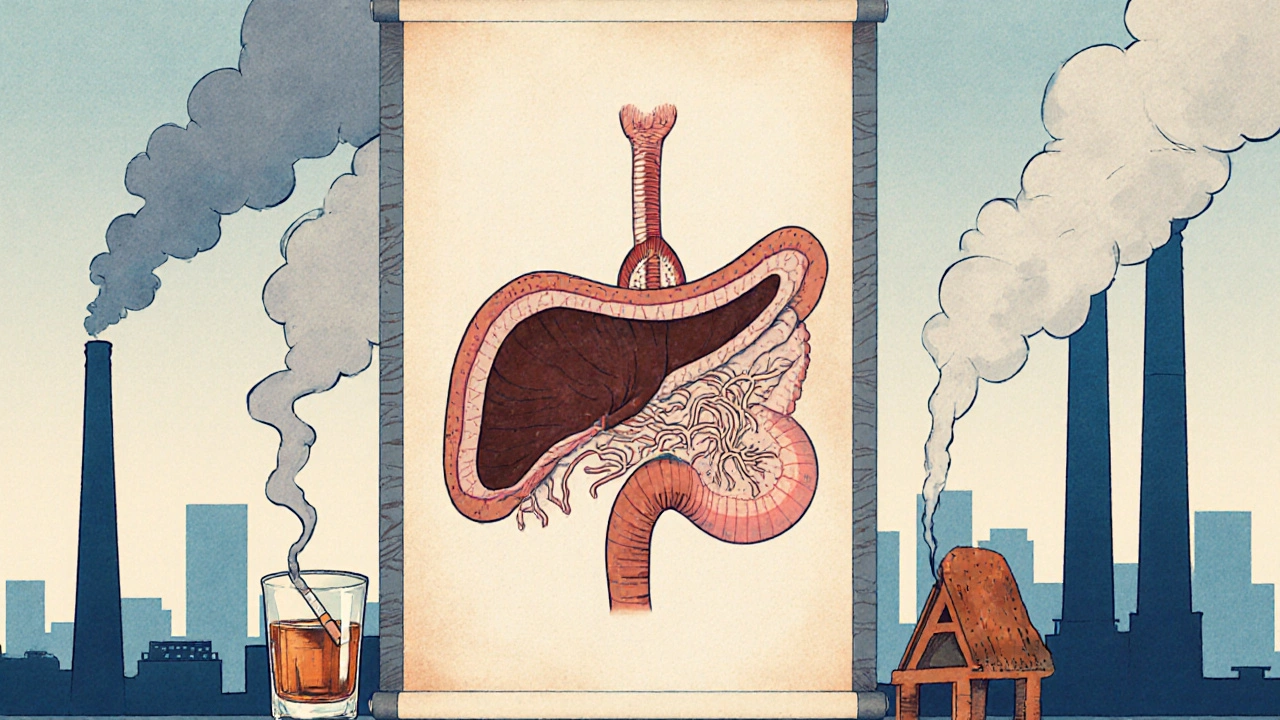
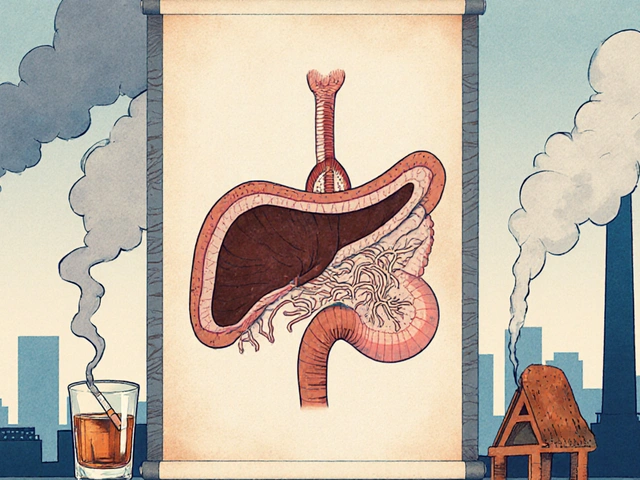
When doctors talk about Pancreatic cancer is a malignant disease that originates in the pancreas, an organ that produces digestive enzymes and hormones. Patients and researchers alike wonder if what we breathe, eat, or work around us can nudge that risk higher. Environmental risk factors are external exposures that may influence disease development, ranging from chemicals to lifestyle habits have been under the microscope for decades. This article pulls together the latest data, separates hype from hard evidence, and gives you practical steps to lower your own odds.
Understanding Pancreatic Cancer
Pancreatic cancer accounts for about 3% of all cancers in the United States but claims roughly 7% of cancer deaths because it is often diagnosed late. The five‑year survival rate hovers around 11%, according to the World Health Organization (WHO). Most tumors arise in the exocrine part of the pancreas, with KRAS gene mutations detected in more than 90% of cases. Early signs-jaundice, unexplained weight loss, or new‑onset diabetes-are vague, which is why early detection strategies focus on high‑risk groups.
How the Environment Can Influence Cancer Risk
Cancer is fundamentally a disease of DNA damage. When cells encounter carcinogens-substances that alter DNA structure-they may acquire mutations that escape normal repair mechanisms. Over time, a cascade of genetic hits can convert a normal pancreatic cell into a malignant one. Environmental exposures act as one of those hits, either directly damaging DNA or creating chronic inflammation that fosters a tumor‑friendly environment.
Key Environmental Factors and What the Evidence Says
Below is a quick glance at the most studied exposures and how strongly they are linked to pancreatic cancer.
| Risk Factor | Evidence Grade | Typical Exposure |
|---|---|---|
| Smoking | Strong | Cigarette smoke, cigars, pipe tobacco |
| Heavy Alcohol Use | Moderate | >3 drinks/day (men), >2 drinks/day (women) |
| Obesity (BMI ≥ 30) | Strong | Excess body fat, especially visceral |
| Type 2 Diabetes | Strong | Chronic hyperglycemia, insulin resistance |
| Industrial Chemicals (e.g., chlorinated solvents) | Limited | Occupational exposure in manufacturing |
| Air Pollution (PM2.5) | Emerging | Urban living, traffic‑related particles |
| Diet High in Red/Processed Meat | Moderate | Frequent consumption of beef, pork, sausages |
| Pesticide Residues | Limited | Residues on non‑organic produce |
Smoking: The Most Consistent Culprit
Large cohort studies, such as the European Prospective Investigation into Cancer and Nutrition (EPIC), have shown that current smokers carry a 1.5‑ to 2‑fold higher risk of pancreatic cancer compared with never‑smokers. Even former smokers retain a modestly elevated risk for up to ten years after quitting. The carcinogens in tobacco smoke-like nitrosamines-directly damage pancreatic duct cells and promote KR‑RAS mutations.
Alcohol and Pancreatitis: A Dangerous Duo
Heavy alcohol consumption can trigger chronic pancreatitis, a known precursor to cancer. A meta‑analysis of 15 studies found that drinking more than three drinks per day raises pancreatic cancer risk by roughly 20%. The relationship is dose‑dependent, meaning the more you drink, the higher the odds.

Obesity, Diabetes, and Metabolic Syndrome
Excess adipose tissue releases inflammatory cytokines (like IL‑6 and TNF‑α) that create a low‑grade inflammatory environment. This milieu accelerates cellular turnover in the pancreas, increasing the chance for DNA errors. Individuals with a BMI over 30 face a 30% higher risk, while those with long‑standing type 2 diabetes see risk climb another 40%.
Occupational and Industrial Chemicals
Workers in the rubber, oil‑refining, and metal‑working industries may encounter chlorinated solvents, benzene, and aromatic amines. While the data are not uniformly strong, case‑control studies from the International Agency for Research on Cancer (IARC) suggest a possible link, especially when exposure exceeds regulatory limits.
Air Pollution: The New Frontier
Fine particulate matter (PM2.5) can penetrate deep into the lungs and enter the bloodstream, eventually reaching the pancreas. Emerging research from Chinese urban cohorts shows a 10% increase in pancreatic cancer incidence for each 10 µg/m³ rise in annual PM2.5 exposure. Though still early, this suggests that city dwellers may face an added invisible risk.
Dietary Patterns: Red Meat and Processed Foods
High intake of red and processed meats introduces heterocyclic amines (HCAs) and nitrosamines formed during cooking. The Nurses’ Health Study linked a diet rich in these foods to a 15% higher pancreatic cancer risk. Conversely, diets abundant in fruits, vegetables, and whole grains provide antioxidants that may counteract DNA damage.
Pesticide Residues and Agricultural Exposures
Farmers and agricultural workers often handle organophosphate pesticides, which have been implicated in various cancers. A pooled analysis of three U.S. case‑control studies found a modest but statistically significant increase in pancreatic cancer among those with high pesticide exposure scores.
Putting the Pieces Together: What the Numbers Really Mean
When you add up all these factors, lifestyle choices (smoking, alcohol, diet, weight) account for roughly 30‑40% of pancreatic cancer cases worldwide. The remaining portion is a mix of genetics, unmeasured environmental exposures, and random chance. This split underscores that while you can’t control your DNA, you can moderate many external risks.
Practical Steps to Lower Your Risk
- Quit smoking - even cutting back reduces risk; consider nicotine replacement or counseling.
- Limit alcohol to moderate levels - no more than two drinks per day for men and one for women.
- Maintain a healthy weight - aim for a BMI below 25 through balanced diet and regular exercise.
- Screen for diabetes early - manage blood sugar with diet, medication, or lifestyle changes.
- Choose plant‑forward meals - replace red meat with fish, legumes, and plenty of colorful vegetables.
- Reduce exposure to industrial chemicals - use protective equipment at work and follow safety guidelines.
- Support clean‑air initiatives - use air purifiers at home and advocate for stricter emissions standards.
While none of these steps guarantee immunity, they collectively chip away at the modifiable fraction of risk.
Future Directions in Research
Large‑scale genomic studies are now pairing DNA sequencing with detailed exposure histories, a method called exposomics. The goal is to pinpoint which environmental agents trigger specific mutations in pancreatic cells. Meanwhile, the IARC is reviewing new data on air pollution and pesticides, which could shift classification from “possible” to “probable” carcinogen for the pancreas.
Can I get pancreatic cancer if I never smoked?
Yes. About 60‑70% of cases occur in people who have never smoked, highlighting the role of genetics and other environmental factors.
Is there a reliable screening test for early‑stage pancreatic cancer?
Currently, no standard population‑wide test exists. High‑risk groups may receive endoscopic ultrasound or MRI scans, but these are not routine.
How strong is the link between air pollution and pancreatic cancer?
Research is still emerging, but several large cohort studies show a 10‑15% increased risk per 10 µg/m³ rise in PM2.5 exposure.
Does a high‑fat diet directly cause pancreatic cancer?
A diet high in saturated fats can promote obesity and insulin resistance, both of which are established risk factors, but the diet alone isn’t shown to be a direct cause.
Are pesticides a major concern for the general public?
For most consumers, residues on produce are low and regulated. However, occupational exposure or living near heavily treated fields may increase risk.






jessie cole
October 20, 2025 AT 14:10Pancreatic cancer remains one of the most daunting diagnoses in modern medicine.
The article you have provided offers a clear and thorough overview of the current evidence.
It is commendable that the authors separate hype from hard data, thereby guiding readers toward actionable steps.
Understanding that smoking, obesity, and chronic inflammation are key drivers empowers individuals to make meaningful changes.
The linkage between environmental pollutants such as PM2.5 and cancer risk, while still emerging, is presented with appropriate caution.
Likewise, the discussion of occupational chemicals highlights the importance of protective measures in the workplace.
The inclusion of dietary recommendations, such as reducing red meat and increasing plant‑forward meals, aligns with broader nutritional guidelines.
Moreover, the emphasis on early detection for high‑risk groups underscores a proactive approach.
It is also noteworthy that the article acknowledges the role of genetics, reminding us that not all risk is modifiable.
The practical steps listed are concise and feasible for many readers.
In particular, quitting smoking even partially can lead to measurable risk reduction.
Maintaining a healthy weight through balanced diet and regular activity is another cornerstone of prevention.
Screening for diabetes and managing blood sugar levels further diminishes the metabolic contributors to cancer.
Supporting clean‑air initiatives, though a collective effort, can also protect vulnerable populations.
Finally, the call for exposomic research signals a promising direction for future investigations.
In sum, the piece serves as both an informative resource and a motivating guide for those seeking to lower their pancreatic cancer risk.
Kirsten Youtsey
October 21, 2025 AT 17:56While the exposition appears exhaustive, one cannot ignore the subtle omission of satellite‑derived pollutant data that many independent researchers have linked to oncogenesis.
The reliance on conventional cohort studies may be a deliberate veil, concealing the true extent of industrial manipulation.
It is regrettable that the authors elect not to delve into the clandestine funding streams that shape environmental health narratives.
Such selective scholarship, though polished, ultimately serves a limited agenda.
Matthew Hall
October 22, 2025 AT 21:43Man, reading that piece felt like pulling back the curtain on a horror show where the villains are the very air we breathe.
They toss in numbers about PM2.5 like it’s just another seasoning, but guess what? Those tiny particles are the silent assassins whispering mutations into our pancreas.
And the whole “you can’t escape it” vibe? Spot on-unless you’re living in a bunker, the city haze is practically invited to the dinner table.
barnabas jacob
October 24, 2025 AT 01:30Your dramatization, while entertaining, dangerously oversimplifyin a complex etiological matrix.
Epidemiologic evidence, quantified via hazard ratios and confidence intervals, contradicts the notion of a monolithic toxin.
Moreover, the moral panic you invoke distracts from actionable public‑health interventions, such as exposure mitigation protocols.
It's imperative that discourse remain anchored in statistically robust methodology, not sensationalist hyperbole.
Otherwise we risk eroding credibility.
Alex Pegg
October 25, 2025 AT 05:16The article's recommendation to replace red meat with fish comes across as a typical Western soft‑power agenda, pushing a diet that aligns with certain geopolitical narratives.
In reality, many of our farming traditions have long relied on wholesome, locally sourced meats without provoking a cancer surge.
One must question whether the cited studies truly represent the diversity of dietary patterns across the globe.
Blindly adopting these guidelines may inadvertently undermine cultural food sovereignty.
laura wood
October 26, 2025 AT 08:03I hear your concerns about preserving culinary heritage, and it’s important to balance tradition with emerging health insights.
While respecting local food practices, we can still explore ways to incorporate more plant‑based elements without discarding cultural identity.
Community‑driven nutrition programs often succeed by blending tradition with science.
Together, we can foster healthier choices that honor both health and heritage.
Kate McKay
October 27, 2025 AT 11:50Great summary of the key points!
First, quit smoking-every cigarette you skip cuts risk.
Second, watch your alcohol; moderation is key.
Third, stay active; a brisk walk three times a week does wonders.
Finally, get checked regularly.
Small changes add up to big protection.
JessicaAnn Sutton
October 28, 2025 AT 15:36While your enthusiasm is commendable, the reductionist checklist you propose neglects the nuanced interplay of socioeconomic determinants that critically modulate disease risk.
A mere enumeration of lifestyle modifications, devoid of systemic context, borders on intellectual negligence.
It is incumbent upon us to address structural inequities alongside individual behavior.
Only through such comprehensive scrutiny can we aspire to genuine risk reduction.
Israel Emory
October 29, 2025 AT 19:23Indeed, collaboration, compassion, and concerted action are essential, - let us move forward together.