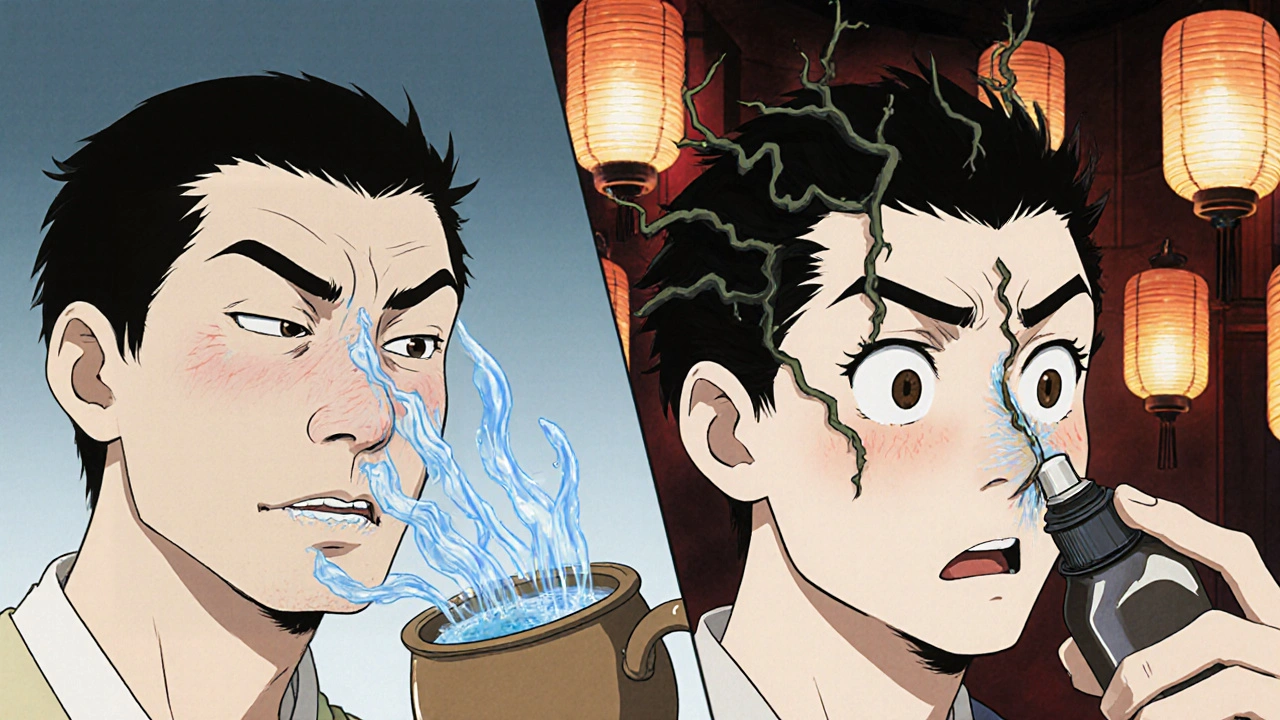
Ever used a nasal spray and felt instant relief-only to have your nose clog up worse than before a few hours later? If you’ve been reaching for that spray every day for more than a few days, you’re not alone. You might be caught in a cycle called rhinitis medicamentosa, or rebound congestion. It’s not just a bad cold or allergies. It’s your nose reacting to the very medicine meant to help it.
What’s Really Going On in Your Nose?
Nasal decongestant sprays like Afrin, Neo-Synephrine, or Vicks Sinex contain active ingredients such as oxymetazoline or phenylephrine. These work by shrinking swollen blood vessels in your nasal passages. That’s why you feel clearer right away. But here’s the catch: your body gets used to it. After three to four days of daily use, the blood vessels stop responding the same way. When the spray wears off, they don’t just return to normal-they overcompensate and swell even more. This is called rebound vasodilation. Your nose becomes dependent on the spray just to stay open.According to the National Center for Biotechnology Information (NCBI), this isn’t rare. About 1 in 10 people who use these sprays beyond the recommended time develop this condition. In the U.S. alone, an estimated 500,000 cases are diagnosed each year. And it’s not just adults-teens and older people are just as likely to fall into this trap, especially if they’re using it for chronic stuffiness from allergies or sinus issues.
Signs you might have rebound congestion:
- Nasal congestion returns or gets worse after the spray wears off
- You feel like you need to spray more often-every 4 to 6 hours instead of every 12
- Your nose feels dry, crusty, or irritated inside
- You’re breathing through your mouth, especially at night
- You’ve been using the spray for more than a week
The nasal lining can look inflamed, red, and bumpy during a doctor’s exam. In long-term cases, the tissue can even thin out and form crusts. Left untreated, chronic overuse increases your risk of nasal polyps-small, noncancerous growths that can block airflow and require surgery.
Why Stopping Feels So Hard
The hardest part isn’t knowing you need to stop-it’s actually doing it. When you quit cold turkey, your congestion can spike. For many, days 2 to 5 are brutal. You might feel like you’re choking, can’t sleep, or get headaches from the pressure. It’s not just discomfort-it’s real physiological withdrawal.One patient on Reddit, who goes by ‘AllergySufferer89’, wrote: ‘After 3 weeks of Flonase and no Afrin, my nose finally cleared up-the first week was hell but worth it.’ That’s the story for most people who make it through. But 18% of users relapse during this time, often because they weren’t prepared for how bad it gets.
That’s why the approach matters. Stopping both nostrils at once can make symptoms worse. Many doctors now recommend a smarter strategy: stop the spray in one nostril first. Wait until that side clears up-usually within a week-then stop it in the other. This halves the shock to your system and makes the withdrawal more manageable.
What Actually Works to Fix It
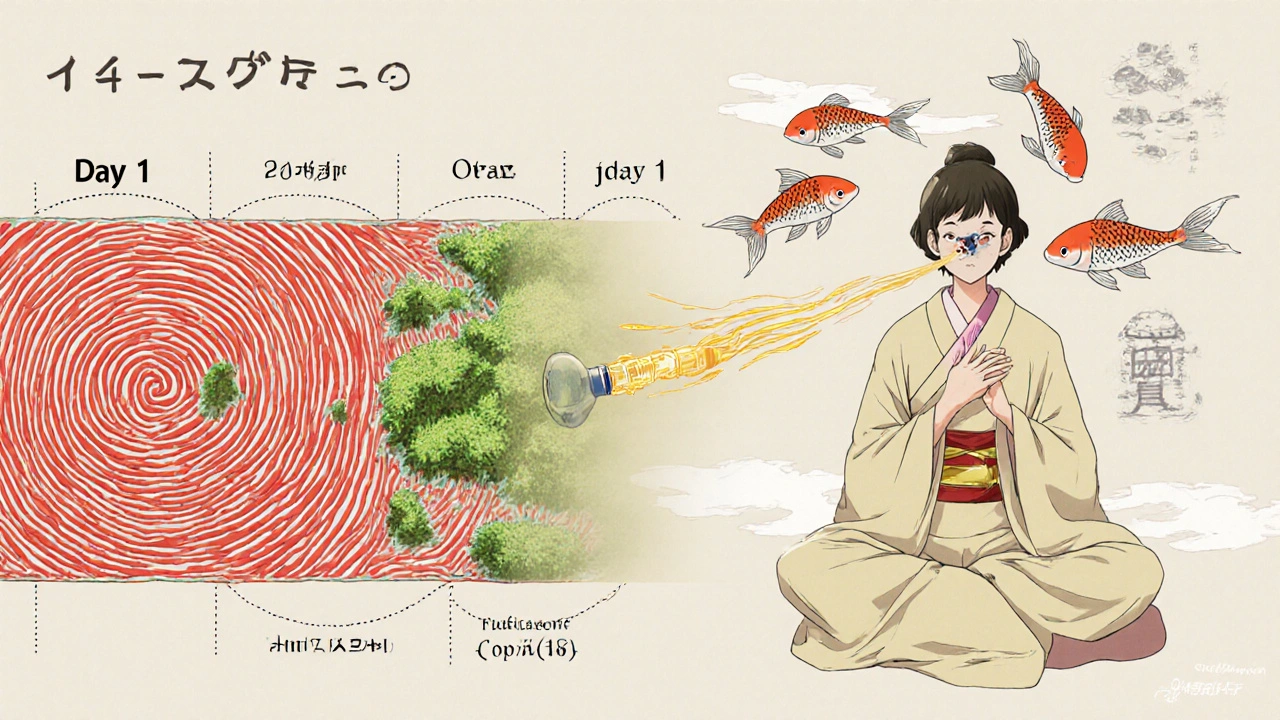
The good news? Rhinitis medicamentosa is reversible. You just need the right tools and patience.1. Intranasal corticosteroids are the gold standard. Medications like Flonase (fluticasone) or Nasonex (mometasone) reduce inflammation without causing rebound. They don’t work right away-it takes 5 to 7 days to start helping, and up to 2 to 4 weeks for full effect. But studies show 68% to 75% of people see major improvement with consistent use. Use them twice daily at first, then once daily as symptoms improve.
2. Saline nasal irrigation is simple, safe, and effective. Rinsing your nose with salt water (using a neti pot or squeeze bottle) clears mucus, soothes irritated tissue, and reduces the urge to spray. A 2022 review in the Journal of Allergy and Clinical Immunology found that 60% of users reported noticeable relief. Do it 2 to 3 times a day during withdrawal.
3. Short-term oral steroids like prednisone can help in severe cases. A 2021 clinical trial showed 82% of patients had significant improvement after a 5-day course at 0.5 mg per kg of body weight. This is usually reserved for people with extreme swelling or those who haven’t responded to other treatments.
4. Avoid triggers. If you’re taking other medications like MAO inhibitors (used for depression), combining them with decongestants can cause dangerous spikes in blood pressure. Even oral decongestants like pseudoephedrine can worsen your condition. Check with your pharmacist before taking anything new.
What Doesn’t Work (and Why)
Some people try to ‘wean off’ by switching to a different brand of nasal spray. That doesn’t help. All topical decongestants work the same way-oxymetazoline, phenylephrine, xylometazoline-they’re all part of the same problem.Antihistamine sprays like azelastine (Astelin) are sometimes used for allergies, but they don’t fix rebound congestion. They might help if allergies are also a factor, but they won’t reverse the dependency cycle.
And no, using more spray isn’t the answer. Each extra drop makes the rebound worse. The FDA now requires all OTC nasal spray packaging to say clearly: ‘DO NOT USE MORE THAN 3 DAYS.’ That’s not a suggestion-it’s science.
How to Prevent It from Happening Again
The best treatment is prevention. Here’s how to avoid falling back into the trap:- Use nasal decongestant sprays for no more than 3 days in a row. Always read the label.
- Start with saline irrigation if you’re congested. It’s just as effective for short-term relief and has zero risk of rebound.
- If congestion lasts longer than a week, see a doctor. You might need allergy testing or treatment for sinusitis.
- Keep a nasal spray diary. Write down when you use it and why. This helps you spot patterns before they become habits.
- Consider switching to a steroid spray if you have chronic congestion. Flonase and Nasacort are safe for daily, long-term use.
Studies show that people who use saline irrigation as their first line of defense cut their risk of rebound congestion by 40%. That’s huge. It’s not glamorous, but it works.
Real Recovery Timeline
Here’s what to expect if you follow the plan:- Days 1-3: Congestion peaks. Use saline rinses every 2-3 hours. Start corticosteroid spray twice daily. Sleep with your head elevated.
- Days 4-7: Gradual improvement. Congestion eases by 30-50%. Keep using corticosteroid once or twice daily. Avoid irritants like smoke or strong perfumes.
- Days 8-14: Significant relief. Most people report 70-90% improvement. Corticosteroid can be reduced to once daily. Your sense of smell may start returning.
- Week 3 and beyond: Normal function returns. Keep using corticosteroid if you have allergies. Never go back to decongestant sprays unless advised by a doctor.
Success rates jump from 63% if you wait 4 weeks to start treatment, to 89% if you act within the first two weeks. Early action saves time, discomfort, and money.
Frequently Asked Questions
Can I use saline spray every day?
Yes. Saline nasal spray or irrigation is safe for daily, long-term use. It doesn’t cause rebound congestion and helps keep nasal passages moist and clear. Use it as often as needed-even multiple times a day-especially during cold season or if you’re in dry air.
How long does rebound congestion last?
Symptoms usually peak within 3-5 days after stopping the spray and improve over 1-2 weeks. Most people feel significantly better by day 14. In rare cases, it can take up to a month, especially if you’ve been using sprays for months or years. Patience and consistent treatment are key.
Is Flonase safe for long-term use?
Yes. Flonase (fluticasone) and other intranasal corticosteroids are designed for daily, long-term use. They reduce inflammation without causing dependency. Unlike decongestant sprays, they don’t shrink blood vessels-they calm the immune response in your nose. Side effects are rare and mild, like slight nosebleeds or dryness.
Can children get rebound congestion from nasal sprays?
Yes. Children are just as susceptible, especially if they’re given adult-strength sprays without supervision. Always use age-appropriate products and follow dosage instructions. For kids under 6, consult a pediatrician before using any nasal spray.
What if my nose is still blocked after 2 weeks?
If you’ve stopped the decongestant spray and used corticosteroids and saline for two weeks with no improvement, see an ENT specialist. You might have underlying issues like nasal polyps, a deviated septum, or chronic sinusitis. These require different treatments, like imaging or surgery.








edgar popa
November 11, 2025 AT 08:52bro i used afrin for 3 weeks straight and thought i was dying. then i stopped cold turkey and cried for 4 days. now i use saline like its my job and my nose is actually happy. no more mouth breathing at night. you got this.
Eve Miller
November 11, 2025 AT 14:03It’s appalling how many people treat OTC nasal decongestants like candy. The FDA warning is there for a reason, and yet, people ignore it until their nasal mucosa resembles a battlefield. This post is a public service.
Chrisna Bronkhorst
November 12, 2025 AT 21:25Rebound congestion isn't even the real problem. The real issue is pharma companies pushing these sprays like they're vitamins. They know people will get hooked. The 3-day limit? A loophole. They want you to buy more. It's a $2B market built on addiction. Wake up.
Amie Wilde
November 13, 2025 AT 12:27Saline saved me. No drama. No side effects. Just water and salt. Why is this not the first thing everyone tries?
Gary Hattis
November 13, 2025 AT 17:33As someone who grew up in a household where grandma swore by saltwater rinses, it’s wild to see how much we’ve forgotten traditional remedies. In India, they’ve used jala neti for centuries. In Mexico, they use saline sprays daily. We’re overcomplicating simple biology. Sometimes the answer isn’t a chemical - it’s just clean water.
Esperanza Decor
November 15, 2025 AT 17:27I started using Flonase after reading this and honestly, I thought it was a scam. But after 10 days, my nose stopped feeling like a desert. I didn’t even realize how much I was mouth-breathing until I could breathe through my nose again. This changed my sleep. My energy. My life.
Deepa Lakshminarasimhan
November 17, 2025 AT 12:08They say it’s rebound congestion… but what if it’s not? What if the sprays are just masking what the CDC is hiding? Why do all the studies come from drug companies? Why is there no long-term independent research? I’m not buying it. They want you dependent. Always.
Erica Cruz
November 17, 2025 AT 23:56Wow. Another self-help post about nasal sprays. So dramatic. People have been using these for decades. You’re acting like it’s a life-or-death crisis. Maybe you just have bad allergies and need to move to a less polluted city. Or stop eating dairy. Or sleep on your side. So many variables, and yet we blame the spray.
Johnson Abraham
November 19, 2025 AT 17:12flonase is just as bad. they just call it different. same chemicals, different name. i tried it. my nose got dry and then i started bleeding. now i just use a humidifier and ignore it. works better anyway lol
Shante Ajadeen
November 21, 2025 AT 11:04I was skeptical too, but I did the one-nostril trick like they said. Day 3 was rough, but day 5? I could breathe. I cried. I didn’t even know how bad it had gotten until I could finally take a full breath. You’re not alone. Keep going.
dace yates
November 23, 2025 AT 05:04Has anyone tried using a neti pot with distilled water and baking soda instead of salt? I heard it’s gentler on the mucosa. Anyone have data on that?
Danae Miley
November 23, 2025 AT 12:23The claim that 68% to 75% of users see improvement with corticosteroids is misleading. The studies cited have small sample sizes and short follow-up periods. Also, ‘major improvement’ is not defined. This is anecdotal evidence dressed as science.
Charles Lewis
November 24, 2025 AT 01:51Let me offer some perspective from my 22 years as a primary care physician. Rebound congestion is one of the most underdiagnosed conditions in outpatient practice. Patients often come in saying, ‘I just can’t breathe,’ and we assume it’s allergies. But when we ask about nasal spray use, it’s almost always the culprit. The real tragedy isn’t the congestion - it’s that patients feel ashamed to admit they’ve been using it daily. We need more compassion, not judgment. And yes - saline irrigation, corticosteroids, and patience are the only reliable path forward. No shortcuts. No magic pills. Just consistent, gentle care.
Renee Ruth
November 25, 2025 AT 19:46I tried stopping for 10 days and ended up in the ER because I couldn’t sleep and my blood pressure spiked. No one warned me. No one told me how dangerous this is. Now I’m on antidepressants because I’m traumatized by my own nose. This post should come with a trigger warning.
Samantha Wade
November 27, 2025 AT 06:52This is one of the most well-researched, compassionate, and actionable pieces I’ve read on this topic in years. Thank you for including the timeline, the science, and the human experience. You’ve given people not just information - you’ve given them hope. Please keep sharing this. It matters more than you know.