Key Takeaways
- RLS in children shows up as an urge to move the legs, especially at night.
- Iron deficiency and dopamine imbalance are the most common biological triggers.
- A simple blood test and sleep‑history interview often confirm the diagnosis.
- Lifestyle tweaks (stretching, good sleep hygiene) work for many; medication is reserved for persistent cases.
- Early recognition prevents sleep loss, daytime fatigue, and academic struggles.
When a child constantly moves their legs or complains of an uncomfortable urge, it could be Restless Leg Syndrome in Children, a neurological sleep‑related condition that triggers an irresistible urge to move the legs, often worsening at night. Unlike the occasional “wiggle‑wiggle” most kids display, RLS lasts for weeks or months, disrupts sleep, and can affect school performance. Below we break down everything a parent, teacher, or pediatric caregiver needs to spot, understand, and manage this condition.
What Exactly Is Restless Leg Syndrome?
Restless Leg Syndrome, a sensorimotor disorder characterized by uncomfortable sensations in the legs and an uncontrollable urge to move them (often abbreviated RLS) is best known in adults. In children, the core features are the same, but the way they express discomfort can differ-some kids describe “creepy‑crawlies,” others simply become fidgety and have trouble staying still.
RLS belongs to a family of sleep‑related movement disorders, alongside Periodic Limb Movement Disorder, a condition where the legs twitch rhythmically during sleep without the conscious urge felt in RLS. While PLMD can coexist with RLS, it lacks the awake‑time discomfort that drives a child to get up and stretch.
How to Spot the Signs
Kids can’t always name the feeling, so watch for behavioral clues:
- Nighttime restlessness: Frequent leg kicking, pacing, or sudden sitting up in bed.
- Complaints of “tingly,” “crawling,” or “painful” legs: Often mentioned when asked about bedtime.
- Improvement with movement: The urge eases after walking, jumping, or stretches.
- Sleep disruption: Difficulty falling asleep, frequent night awakenings, or early morning waking.
- Daytime effects: Irritability, poor attention, or falling behind in school.
If a child shows three or more of these patterns for over a month, it’s time to consider a formal evaluation.

Underlying Causes: Why Do Kids Get RLS?
Most pediatric cases trace back to two main pathways:
- Iron deficiency, low serum ferritin levels that affect dopamine synthesis in the brain. Even a borderline iron level can tip the balance.
- Dopamine dysregulation, an imbalance in the brain’s dopamine signaling that controls movement and sensory perception. This can be genetic or secondary to other medical issues.
Other contributors include:
- Chronic kidney disease or anemia.
- Family history of RLS or related movement disorders.
- Certain medications (e.g., antihistamines, some antidepressants).
- Pregnancy in adolescent females-a less common but documented trigger.
Because iron is a key co‑factor for dopamine production, labs that show low ferritin often point directly to the root cause.
How Doctors Diagnose RLS in Children
The diagnostic process blends history, physical exam, and targeted tests:
- Sleep‑history interview: Parents answer standardized questions about bedtime behavior, leg sensations, and family patterns.
- Physical examination: A pediatrician or Pediatric Neurologist, a doctor who specializes in the nervous system of children checks for neurologic deficits that might mimic RLS.
- Laboratory tests: Serum ferritin, iron, total iron‑binding capacity, and sometimes vitaminD levels.
- Polysomnography (optional): An overnight sleep study that records leg movements, brain waves, and oxygen levels. It’s most useful when the diagnosis is unclear or PLMD is suspected.
There’s no single “RLS scan,” but the combination of a consistent symptom pattern and low ferritin often clinches the diagnosis.
Treatment Options: From Simple Tweaks to Medication
Management follows a step‑wise approach, starting with the least invasive interventions.
1. Lifestyle and Home Strategies
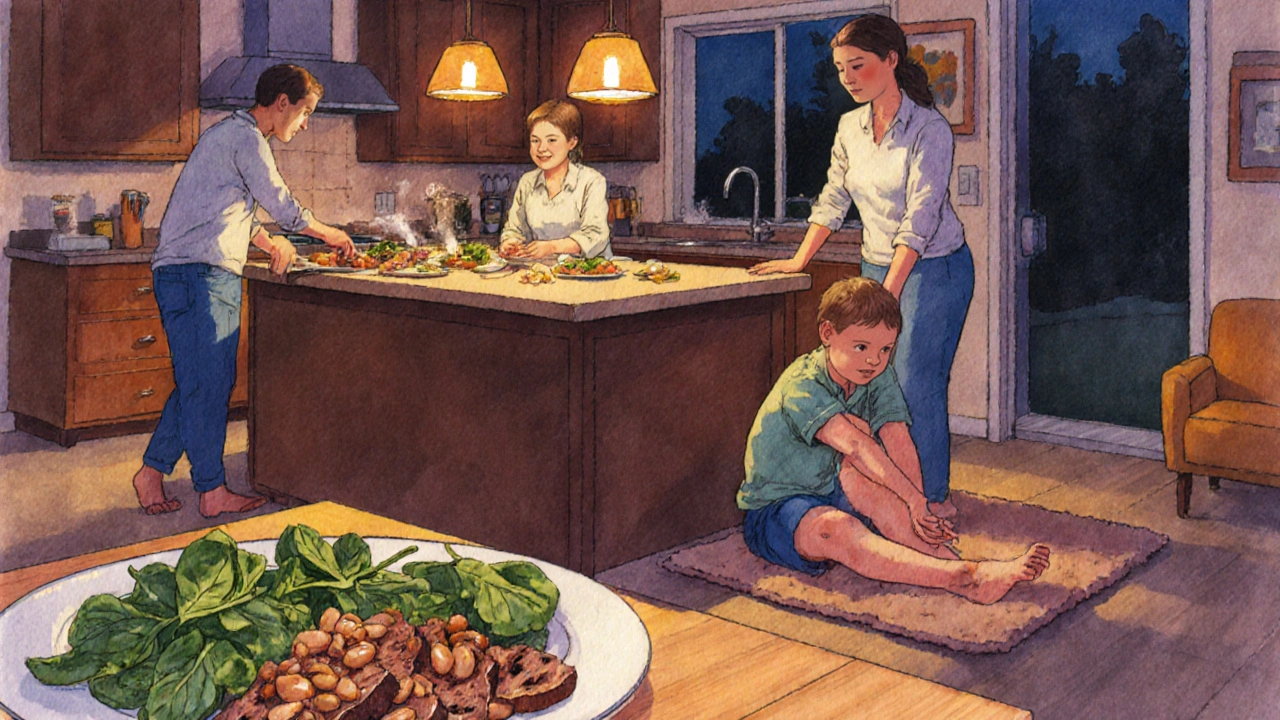
- Iron‑rich diet: Include lean red meat, beans, spinach, and fortified cereals. Pair with vitaminC to enhance absorption.
- Iron supplementation: If ferritin is below 50µg/L, a pediatrician may prescribe low‑dose ferrous sulfate (3‑6mg/kg/day) for 3-6months.
- Good sleep hygiene: Consistent bedtime, a cool dark room, and limiting screen time 1hour before sleep.
- Evening stretching routine: Gentle calf‑muscle stretches or yoga poses (e.g., child’s pose) can reduce the urge.
- Warm baths or heating pads: Warmth often relaxes the sensory nerves.
2. Pharmacologic Choices (When Needed)
Medication is reserved for children who still have significant night‑time symptoms after 4-6weeks of lifestyle changes.
| Medication | Typical Dose | How It Works | Key Side Effects |
|---|---|---|---|
| Low‑dose Dopamine Agonist (e.g., pramipexole) | 0.125mg at bedtime | Enhances dopamine signaling, reducing leg sensations | Nausea, mild dizziness, rare impulse‑control issues |
| Gabapentin | 10‑15mg/kg nightly | Modulates calcium channels, soothing nerve hyper‑excitability | Sleepiness, weight gain |
| Iron Supplement (if ferritin <50µg/L) | 3‑6mg/kg/day elemental iron | Replenishes iron stores, indirectly normalizing dopamine | Stomach upset, constipation |
All meds require close monitoring by a Pediatric Neurologist, to adjust dose and watch for side effects. Regular follow‑up labs ensure iron levels stay in the therapeutic range.
3. Managing Co‑Existing Conditions
If the child has ADHD, anxiety, or chronic pain, treating those issues can also lessen RLS severity. Collaborative care with a child psychologist or a pediatrician ensures a holistic plan.
Preventing Relapse and Long‑Term Outlook
RLS can wax and wane. Here’s how to keep symptoms at bay:
- Annual ferritin check for kids with a history of low iron.
- Maintain a balanced diet rich in iron and vitaminB12.
- Keep a consistent bedtime routine, even on weekends.
- Monitor growth spurts; rapid growth sometimes spikes RLS symptoms.
- Educate teachers and coaches about the child’s condition so they can accommodate restful breaks during the day.
Most children outgrow the condition by late adolescence, especially when iron levels are stable and sleep habits are good. Early intervention, however, prevents the cascade of sleep deprivation, mood swings, and academic setbacks.
Frequently Asked Questions
Can RLS be diagnosed without a sleep study?
Yes. For most children, a thorough sleep‑history interview combined with low ferritin levels is enough. Polysomnography is only needed when symptoms overlap with other sleep disorders.
Is iron supplementation safe for all kids with RLS?
Supplementation is safe when ferritin is below 50µg/L. Excess iron can be harmful, so dosing should be guided by a pediatrician and monitored with follow‑up labs.
Do dopamine agonists cause growth issues?
Low‑dose agents like pramipexole have not been linked to growth suppression in children, but they can cause nausea or mild dizziness. Regular check‑ins help catch any side effects early.
Can diet alone cure RLS?
If iron deficiency is the sole trigger, correcting the deficiency often relieves symptoms. When dopamine dysregulation or genetic factors are involved, diet helps but may need to be paired with other treatments.
Should I wake my child when they get up at night?
Gently encourage them to do a short stretch or walk back to bed. Avoid turning on bright lights; keeping the environment dim helps maintain melatonin production.








Yassin Hammachi
October 10, 2025 AT 20:48RLS in kids often slips under the radar because parents attribute restlessness to typical childhood energy.
The urge to move the legs, especially at night, can be a silent thief of deep sleep.
When the brain lacks sufficient iron, dopamine pathways get shaky, and the sensation of crawling bugs emerges.
That’s why a simple ferritin test can be the first clue a pediatrician looks for.
Beyond iron, genetic factors may predispose a child to dopamine dysregulation, making family history a useful piece of the puzzle.
In practice, asking the child how their legs feel at bedtime can reveal “tingly” or “creepy‑crawlies” descriptors.
If the child reports relief after stretching or walking, that’s a classic hallmark of RLS.
Nighttime pacing, frequent leg kicking, or suddenly sitting up are behavioral red flags.
The downstream effects include irritability, trouble focusing in school, and a cascade of daytime fatigue.
Lifestyle tweaks-like iron‑rich foods, consistent sleep schedules, and evening stretching-often bring noticeable improvement.
Warm baths or a heating pad can calm the sensory nerves before lights‑out.
When these measures fail after several weeks, a low‑dose dopamine agonist such as pramipexole may be considered, but only under careful supervision.
Parents should monitor for side effects like nausea or rare impulse‑control issues.
Ultimately, early recognition and a step‑wise approach protect the child’s sleep hygiene and academic performance.
Keeping open communication with the child and the healthcare team makes managing RLS a collaborative effort.
Michael Wall
October 13, 2025 AT 04:22Honestly, if a kid keeps tossing and turning because of leg twitching, you better get them checked sooner rather than later. Simple blood work can spot iron deficiency, and that’s often the root cause. Don’t just chalk it up to “being hyper” – it’s a real medical issue. Parents should act responsibly and follow the doctor’s advice.
Christopher Xompero
October 15, 2025 AT 11:55Okay, lemme tell ya, i’ve read every article out there on this and i can srsly say you’re missing the drama here. Kids don’t just “wiggle‑wiggle” – it’s a full‑blown nighttime rebellion! The iron deficiency thing? Yeah, sure, but what about the hidden toxins in the water supply? Wake up, people, it’s a conspiracy of “normal” symptoms being ignored!
Irene Harty
October 17, 2025 AT 19:28One must question the legitimacy of these so‑called “simple” remedies. The medical establishment frequently downplays the potential iatrogenic effects of dopamine agonists, which may serve ulterior pharmaceutical interests. Proceed with utmost caution.
Jason Lancer
October 20, 2025 AT 03:02Wow, another “just take iron” suggestion. Yeah, great, but what if the kid’s diet already has iron? Do we just flood them with pills until they turn green? I feel like we’re just tossing a band‑aid over a deeper problem. Maybe we should look at overall nutrition and stress factors instead of a single mineral.
Brooks Gregoria
October 22, 2025 AT 10:35All this talk about diet and sleep hygiene is just soft‑core candy‑coating the fact that many of these cases could be handled with a low‑dose dopamine agonist from the start. Why waste weeks on “stretching” when a precise pharmacologic protocol exists? The hesitancy is only because some doctors fear the stigma.
tierra hopkins
October 24, 2025 AT 18:08Hey, I get that medication can be effective, but let’s not forget how much of a difference consistent bedtime routines and a balanced diet can make. Encouraging kids to do gentle calf stretches before sleep has actually helped a few families I know. Small changes, big impact.
Ryan Walsh
October 27, 2025 AT 00:42Totally agree with the stretching tip. I’ve also found that limiting screen time at least an hour before bed and keeping the room cool can calm the nervous system. If you pair that with iron‑rich foods like spinach and beans, many kids see improvement without needing meds.
Kiersten Denton
October 29, 2025 AT 08:15Sounds like a solid plan.
Karl Norton
October 31, 2025 AT 15:48Honestly, this “natural” approach is overrated. Parents keep waiting for miracle foods while the child’s sleep gets wrecked. If the simple diet tweak doesn’t work in a month, you’re just prolonging suffering. Time to be pragmatic and consider medical options.
Ashley Leonard
November 2, 2025 AT 23:22Great points! I’m curious, though – have any of you noticed a correlation between vitamin D levels and RLS severity? Some studies hint at a link, and checking vitamin D might give another piece of the puzzle. Just something to keep in mind when ordering labs.
Ramanathan Valliyappa
November 5, 2025 AT 06:55Correction: The standard reference range for serum ferritin in children is 12‑300 µg/L, not the adult range often cited. Also, “low‑dose” pramipexole typically starts at 0.125 mg, not 0.5 mg. Accuracy matters.
lucy kindseth
November 7, 2025 AT 14:28Thanks for the lab clarification! For families looking to boost iron naturally, adding a vitamin C source like orange juice with meals can really help absorption. Also, be mindful of calcium‑rich foods right after iron supplements, as they can hinder uptake.
Nymia Jones
November 9, 2025 AT 22:02It is worth noting that the pharmaceutical industry has a vested interest in promoting dopamine agonists, subtly influencing clinical guidelines. Independent research suggests that lifestyle interventions have comparable outcomes without the hidden costs. One must remain vigilant.
Karen McCormack
November 12, 2025 AT 05:35Imagine the restless legs as tiny philosophers, constantly questioning the stillness of the night. When they’re ignored, they protest with kicks and twitches, demanding acknowledgment. By feeding them iron and soothing routines, we’re essentially offering them a cup of philosophical tea, allowing them to contemplate in peace.
Rene Lacey
November 14, 2025 AT 13:08The interplay between iron metabolism and dopamine synthesis is a fascinating cascade that underscores how microscopic deficiencies can manifest as macroscopic behavioral patterns. When a child experiences that unsettling urge to move, it’s not merely a nuisance; it’s a neurochemical signal pleading for balance. Addressing it through both nutritional and behavioral lenses acknowledges the holistic nature of pediatric health. Moreover, the feedback loop between sleep quality and daytime cognition cannot be overstated, as chronic disruption may impair learning trajectories. By integrating lab assessments with empathetic bedside discussions, clinicians foster trust and empower families. In sum, a comprehensive, stepwise strategy honors both the science and the lived experience of the child.
johnson mose
November 16, 2025 AT 20:42Wow, that was a deep dive! I’ve seen kids bounce back dramatically once the iron levels were corrected and the bedtime routine tightened. It really shows that sometimes the simplest tweaks-like a warm bath or a quick stretch-can be the hero of the story. For anyone on the fence, give the lifestyle changes a solid month before thinking about meds.
Charmaine De Castro
November 19, 2025 AT 04:15Appreciate all the shared experiences. It’s reassuring to know that a collaborative approach-combining diet, sleep hygiene, and careful medical oversight-can make a real difference for kids dealing with restless leg syndrome.