When you’re dealing with unexpected leaks or a constantly‑full feeling, the first question is usually, “What’s wrong with my bladder?” The answer often lies in a set of specialized exams called urodynamic testing is a group of measurements that evaluate how the bladder stores and releases urine, helping clinicians pinpoint the cause of incontinence or other urinary complaints. This article walks through why these tests matter, what each one looks at, and how the results guide treatment decisions.
Quick Takeaways
- Urodynamic testing provides objective data on bladder pressure, flow, and muscle activity.
- Cystometry is the core test; it maps bladder capacity and sensation.
- Pressure‑flow studies differentiate obstruction from weak muscle contractility.
- Uroflowmetry and EMG add useful clues without invasive catheters.
- Understanding test results helps match patients with the right therapy - from pelvic‑floor exercises to surgery.
Why Simple Questionnaires Aren’t Enough
Patients often describe symptoms in vague terms: “I keep leaking when I cough,” or “I feel like I can’t fully empty my bladder.” Those clues are valuable, but they can’t tell you whether the leak is caused by an overactive detrusor muscle, a weak urethral sphincter, or an anatomical blockage. Without objective measurements, doctors may trial‑and‑error treatments that waste time and money.
Urodynamic testing fills that gap by converting sensations into numbers. The International Continence Society (ICS) recommends these studies whenever the diagnosis is uncertain, before surgery, or when symptoms are severe enough to affect quality of life.
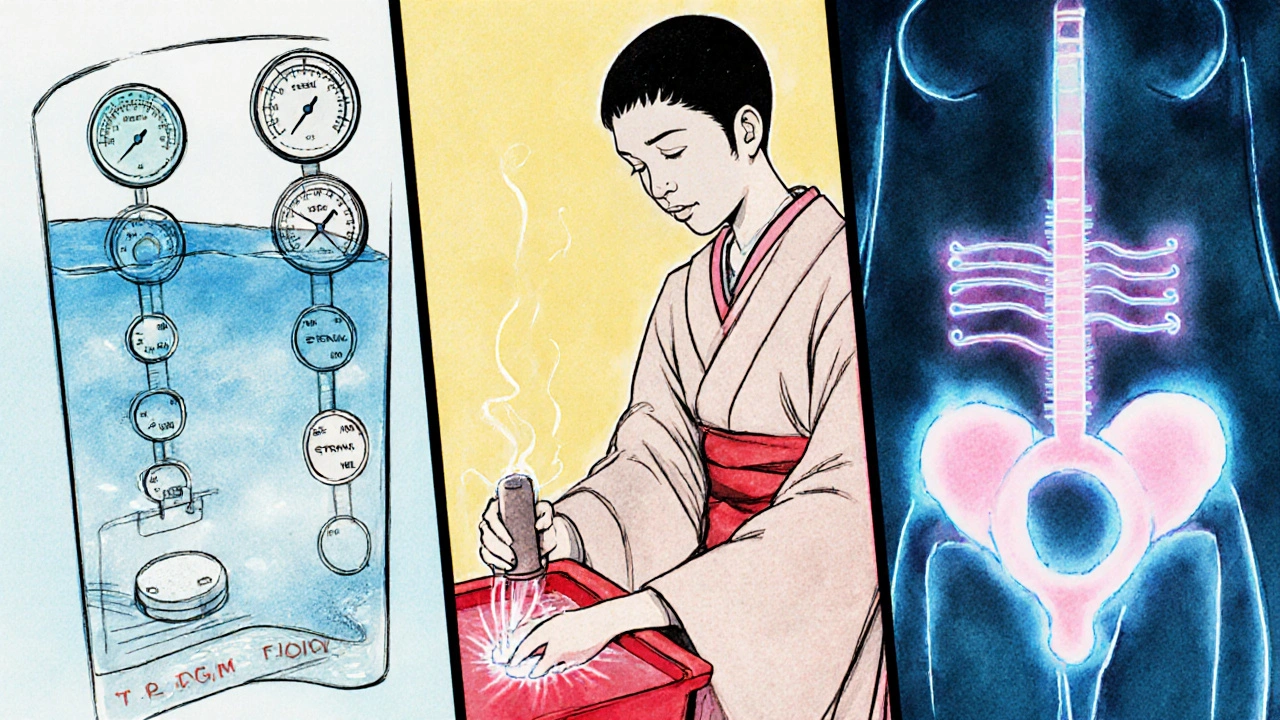
Core Components of a Urodynamic Study
Most clinics run a standard series of tests in a single appointment. Below is a brief look at each component and what it reveals.
- Cystometry (capacity test): A thin catheter fills the bladder with sterile water while pressure sensors record intravesical pressure. The patient reports the first urge, normal urge, and strong urge. The curve shows bladder compliance and detrusor overactivity.
- Pressure‑flow study: After the bladder reaches a comfortable volume, the patient is asked to void. Simultaneous measurement of detrusor pressure and urine flow rate identifies obstruction (high pressure, low flow) versus weak muscle (low pressure, low flow).
- Uroflowmetry: A non‑invasive flow meter placed under the toilet measures peak flow, average flow, and voided volume. It’s quick and helps flag a possible obstruction before more invasive steps.
- Electromyography (EMG): Surface or needle electrodes record activity of the external urethral sphincter during filling and emptying. Abnormal EMG patterns point to neurogenic problems or sphincter dysfunction.
- Video urodynamics (optional): Fluoroscopy images the bladder and urethra while the other tests run, revealing anatomical causes like diverticula or urethral strictures.
Comparing the Most Common Urodynamic Tests
| Test | Primary Purpose | Key Metric(s) | Typical Indication |
|---|---|---|---|
| Cystometry | Assess bladder capacity and sensation | First urge volume, maximum cystometric capacity, detrusor overactivity | Unexplained urgency, mixed incontinence |
| Pressure‑flow study | Separate obstruction from weak detrusor | Detrusor pressure at Qmax, maximum flow rate (Qmax) | Low‑flow voiding, post‑void residual >100 mL |
| Uroflowmetry | Screen for flow abnormalities | Peak flow, average flow, voided volume | Routine assessment, pre‑operative check |
| Electromyography | Evaluate sphincter muscle activity | EMG amplitude, timing of contraction/relaxation | Neurogenic bladder, stress incontinence |
| Video urodynamics | Visualize anatomy during filling/voiding | Fluoroscopic images, simultaneous pressure data | Complex cases, suspicion of anatomic obstruction |
Interpreting Results for Common Incontinence Types
Once the data are collected, a continence specialist matches patterns to clinical categories.
- Stress urinary incontinence (SUI): Usually shows normal cystometric capacity, low‑pressure during filling, but EMG may reveal a weak sphincter burst during coughing.
- Urge urinary incontinence (UUI): Characterized by detrusor overactivity on cystometry - involuntary contractions before the bladder reaches normal capacity.
- Mixed incontinence: Both SUI and UUI findings appear; treatment often combines pelvic‑floor strengthening with bladder‑training medications.
- Overflow incontinence: Low flow rates with high post‑void residual; pressure‑flow study shows a high detrusor pressure but insufficient flow, suggesting obstruction or underactive muscle.
These objective clues are why urodynamic testing is called the “gold standard” for complex or refractory cases. They also help avoid unnecessary surgery - for example, a patient with pure SUI may benefit from a mid‑urethral sling, while a patient with significant detrusor overactivity might need anticholinergic medication first.
When to Order Urodynamics - Practical Checklist
- Symptoms are severe (≥2 episodes per day) or greatly affect daily life.
- Initial treatment (behavioral, pelvic‑floor, medication) has failed after 3-6 months.
- Surgery is being considered - the surgeon needs baseline data.
- There is a history of neurological disease (multiple sclerosis, spinal injury) that could cause neurogenic bladder.
- Unexplained high post‑void residual despite normal physical exam.
If a patient meets any of these triggers, a referral to a continence clinic for a full urodynamic work‑up is warranted.
Preparing for the Test - What Patients Should Know
Good preparation improves test accuracy and comfort.
- Stop drinking caffeine and alcohol 24 hours before.
- Arrive with a comfortably full bladder - usually the clinic will ask you to drink 500 ml of water 30 minutes prior.
- Avoid heavy bladder‑irritating foods (spicy, citrus) the day of the appointment.
- Bring a list of current medications, especially diuretics, anticholinergics, and alpha‑blockers.
- Wear loose‑fitting clothing for easy catheter insertion.
The procedure typically lasts 30-45 minutes. Catheters are thin and may cause mild discomfort, but most patients tolerate them well.

Potential Pitfalls and How to Avoid Misinterpretation
Even with objective data, clinicians can slip into common traps.
- Over‑reliance on a single metric: A low Qmax alone does not confirm obstruction; you must pair it with detrusor pressure.
- Ignoring patient‑reported sensations: The subjective urge scores during cystometry guide diagnosis of overactivity.
- Failing to repeat tests when results are borderline: Some patients have variable bladder behavior; a repeat study can clarify.
- Not considering comorbidities: Diabetes, pelvic surgery, or prostate enlargement alter bladder dynamics and may skew results.
By cross‑checking each data point with the clinical picture, clinicians formulate a nuanced plan rather than a one‑size‑fits‑all solution.
Future Directions - What’s Coming in Urodynamics?
Technology is moving faster than ever. Portable, catheter‑free devices using ultrasound bladder scanning are being validated for flow measurement, potentially reducing invasiveness. Artificial‑intelligence algorithms are already being trained on thousands of pressure‑flow curves to predict outcomes of sling surgery with 85 % accuracy. While these advances won’t replace the need for detailed studies today, they promise quicker screening and more personalized treatment pathways.
Bottom Line
If you or someone you know is battling frequent leaks or a feeling of incomplete emptying, urodynamic testing can turn vague complaints into clear numbers. Those numbers guide whether the next step is pelvic‑floor therapy, medication, or a surgical option. Asking your urologist or continence nurse about a full urodynamic work‑up is a proactive move toward lasting relief.
What does a cystometry test measure?
Cystometry records bladder pressure while it fills with water, capturing the volumes at first urge, normal urge, and strong urge, as well as any involuntary detrusor contractions.
Is urodynamic testing painful?
Most patients experience mild discomfort when a thin catheter is inserted, but the procedure is generally well‑tolerated. Local anesthetic gel can be applied if needed.
How long does it take to get results?
A urodynamic study is interpreted immediately after the test session; a written report is usually available within a few days for the referring physician.
Can urodynamic testing predict success of sling surgery?
Yes. A normal leak point pressure and intact sphincter EMG pattern correlate with higher sling‑surgery success rates, while significant detrusor overactivity may suggest the need for adjunctive medication.
Do I need to fast before the test?
You don’t need a full fast, but avoiding caffeine, alcohol, and large fluid loads the night before helps produce stable baseline measurements.







Jen Taylor
October 22, 2025 AT 22:18Okay, I’ve had two urodynamic tests-and honestly? The first time I was terrified. But the catheter? Thinner than my eyelash curler. The real shocker? Learning my bladder has a ‘strong urge’ at 250ml, not 400 like I thought. My pelvic floor PT cried tears of joy when she saw the cystometry curve. Finally, a reason for my 3am bathroom marathons.
Also-STOP drinking coffee at 4pm. I know you think it’s ‘just one cup.’ It’s not. It’s a betrayal.
And yes, the EMG felt like tiny electric ants. But worth it.
Shilah Lala
October 23, 2025 AT 17:47So we pay $2,000 to stick tubes in our private parts so a doctor can tell us what we already knew: ‘You pee too much.’
Meanwhile, my grandma in Ohio just drinks cranberry juice and calls it a day. Maybe the real diagnosis is ‘modern medicine overcomplicating the human body.’
Christy Tomerlin
October 24, 2025 AT 12:54U.S. healthcare is a circus. You need a PhD to understand why your bladder misbehaves. In India, they just say ‘drink warm water’ and move on. No catheters. No graphs. Just life.
Also-why do Americans need a flow meter to know when they need to pee? You’re not a robot.
Susan Karabin
October 24, 2025 AT 13:19It’s wild how we’ve turned something so natural into a science experiment
Bladder isn’t a machine, it’s a conversation between your body and your brain
Maybe the real issue isn’t the test-it’s that we’ve forgotten how to listen to ourselves
I used to hold it until my knees shook. Now I just go. And guess what? My bladder didn’t explode
Maybe the cure isn’t more data-it’s less guilt
Also, I drank the 500ml water before the test. Felt like a water balloon with legs
But hey-I got answers. And that’s enough for now
Lorena Cabal Lopez
October 25, 2025 AT 00:04These tests are overkill. If you leak when you sneeze, do a Kegel. Done. No need for electrodes, pressure readings, or fluoroscopy. You’re not a NASA rocket.
Also, why is this even covered by insurance? It’s just a fancy way to charge people for discomfort.
Stuart Palley
October 25, 2025 AT 16:17I had this done last year and let me tell you-it’s not the catheter that hurts, it’s the silence while they stare at the screen like they’re decoding the meaning of life
And then they say ‘you have detrusor overactivity’ like it’s a tattoo you got at 19
My urologist didn’t even look me in the eye. Just nodded at the graph like it was a horoscope
Also, I cried. Not because of pain. Because I realized I’d been living with this for 12 years and no one ever asked me how it made me feel
So yeah. It’s invasive. But it’s also the first time I felt seen
Glenda Walsh
October 26, 2025 AT 02:45Wait-so you’re telling me I can’t just drink less water? 😭 I’ve been trying to ‘train’ my bladder for months by holding it longer and now I find out I need a catheter to prove I’m not crazy?
Also, can we talk about how weird it is that we have to pee on a special toilet with sensors? Like, why not just use my own toilet? Do they think I’m lying about my flow rate? 😑
And why do they make you wear those paper gowns? I felt like a confused potato.
Also-did anyone else get the ‘urge’ during the test and the nurse said ‘nope, keep going’? I nearly jumped out of the chair.
Also-can we get a version of this without the catheter? Like, a Bluetooth bladder? 😅
Tanuja Santhanakrishnan
October 26, 2025 AT 23:57As someone from India who’s seen both systems, I can say this: the U.S. approach is thorough, but it’s also expensive. In rural clinics here, we use simple tools-like measuring post-void residual with a handheld ultrasound. No catheter needed. And guess what? It works.
But I love how this article breaks down the science. The table comparing tests? Perfect. I shared it with my sister who’s been struggling with mixed incontinence.
Also-yes, caffeine is the enemy. I quit it for 3 weeks and my nighttime trips dropped from 5 to 1. No magic, just biology.
And to the person who said ‘just drink warm water’-it helps, but it’s not enough for everyone. Urodynamics isn’t overkill. It’s dignity.
One test. One truth. One life changed.
Raj Modi
October 27, 2025 AT 11:54It is imperative to underscore the scientific rigor underpinning the urodynamic assessment protocol, as it represents a cornerstone in the evidence-based management of lower urinary tract dysfunction. The integration of cystometry, pressure-flow analysis, and electromyography provides a multidimensional diagnostic framework that transcends the limitations of subjective symptom reporting. Furthermore, the inclusion of video urodynamics in complex cases allows for the precise delineation of anatomical anomalies that may otherwise remain occult. The International Continence Society’s recommendations are not merely guidelines but clinical imperatives, particularly in the context of preoperative planning for surgical interventions such as mid-urethral sling placement. It is noteworthy that the correlation between objective urodynamic parameters and surgical outcomes has been validated in multiple prospective cohort studies, thereby reinforcing the necessity of this modality in refractory cases. Moreover, the avoidance of premature surgical intervention in patients with neurogenic bladder or detrusor underactivity is a critical safeguard against iatrogenic morbidity. The future integration of AI-driven pattern recognition into urodynamic interpretation promises to enhance diagnostic accuracy and personalize therapeutic algorithms, thereby heralding a new epoch in continence care. Therefore, clinicians must prioritize comprehensive urodynamic evaluation whenever clinical ambiguity persists, as the cost of omission far outweighs the temporary discomfort of the procedure.
Cecil Mays
October 28, 2025 AT 04:30Just had my first urodynamic test and I’m walking out with a new lease on life 🙌
Turns out I didn’t have a ‘weak bladder’-I had a ‘confused bladder’ that thought it was in a rock concert and needed to scream every 20 minutes 😅
Now I’m doing my Kegels like a boss, cutting out soda, and actually listening to my body instead of ignoring it until it screams.
Also-yes, the catheter felt weird. But the relief? Worth every second.
To anyone scared to get tested: you’re not broken. You’re just waiting for the right data to take back your life. 💪🩺
And hey-if you’re reading this, go talk to your doc. You’ve got this. 🌟