Chronic Obstructive Pulmonary Disease, or COPD, isn't just a cough that won't go away. It's a progressive lung condition that slowly steals your ability to breathe normally. By 2025, over COPD affects nearly 400 million people worldwide, and it's the third leading cause of death globally. Many people don't realize they have it until their lungs are already significantly damaged. The good news? If caught early, you can slow it down - and live better, longer.
What Exactly Is COPD?
COPD isn’t one single disease. It’s an umbrella term for two main conditions: chronic bronchitis and emphysema. Chronic bronchitis means your airways are inflamed and produce too much mucus, making you cough constantly. Emphysema damages the air sacs in your lungs, so they can’t hold air properly. Both make it harder to get oxygen in and carbon dioxide out.
The biggest cause? Smoking. About 85 to 90% of cases are directly linked to cigarette smoke. But it’s not just smokers. Long-term exposure to air pollution, chemical fumes, dust, or secondhand smoke can also trigger it. In some rare cases, a genetic condition called alpha-1 antitrypsin deficiency plays a role.
There’s no cure. But that doesn’t mean nothing can be done. Treatment focuses on managing symptoms, preventing flare-ups, and keeping you active. The key is catching it early - before you’ve lost too much lung function.
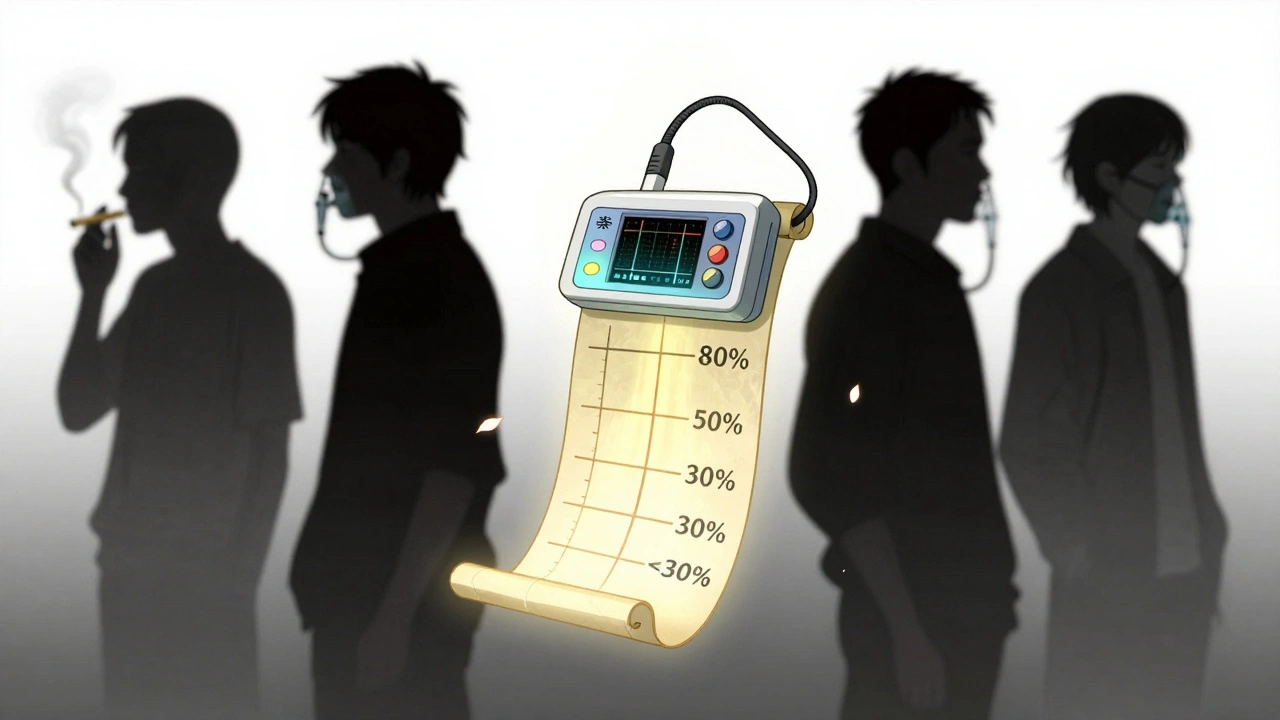
The Four Stages of COPD: From Mild to Very Severe
COPD is staged using a system called GOLD (Global Initiative for Chronic Obstructive Lung Disease), updated in 2023. It’s not just about how bad your breathing feels - it’s measured by a simple test called spirometry. This test measures how much air you can forcefully blow out in one second (FEV1), compared to what’s normal for someone your age, height, and gender.
Stage 1: Mild COPD (FEV1 ≥ 80%)
At this stage, you might not even know you have COPD. You could have a persistent morning cough with phlegm, or get winded after climbing stairs or running to catch the bus. Most people brush it off as being out of shape or aging. But if you’ve smoked for years and have these symptoms, it’s worth getting checked. The good news? Quitting smoking now can cut disease progression by half.
Stage 2: Moderate COPD (FEV1 50-79%)
Breathlessness becomes harder to ignore. Walking at a normal pace makes you stop and catch your breath. You might find yourself avoiding social events because you’re too tired. This is the stage where most people finally get diagnosed. Spirometry confirms it. Treatment usually starts with long-acting inhalers like tiotropium or salmeterol. Pulmonary rehab - a program with exercise training, breathing techniques, and education - can improve your walking distance by over 50 meters in just 8 weeks.
Stage 3: Severe COPD (FEV1 30-49%)
Everyday tasks become exhausting. Getting dressed, cooking a meal, or even showering leaves you gasping. You’re likely having flare-ups (exacerbations) two or more times a year, sometimes needing antibiotics or steroids. Oxygen levels may start dropping during activity. Doctors often add inhaled steroids to your regimen if you’re having frequent flare-ups. Supplemental oxygen might be needed during sleep or exertion.
Stage 4: Very Severe COPD (FEV1 < 30%, or < 50% with chronic respiratory failure)
This is end-stage COPD. You’re short of breath even at rest. Many rely on portable oxygen tanks 15+ hours a day. Simple movements like brushing your teeth can trigger panic. Some develop blue lips or fingernails (cyanosis), confusion from low oxygen, or heart strain. At this point, lung volume reduction surgery or even transplant may be considered - but only for younger, otherwise healthy patients. The focus shifts to comfort, quality of life, and preventing hospitalizations.
Treatment Options by Stage
Treatment isn’t one-size-fits-all. It changes as your disease progresses.
Stage 1: Prevention Is Key
If you smoke - stop. That’s the single most effective thing you can do. No medication can match the benefit of quitting. Short-acting inhalers like albuterol can help during sudden breathlessness. Flu and pneumonia vaccines are critical. Most people at this stage don’t need daily meds - just awareness and action.
Stage 2: Keeping You Moving
Long-acting bronchodilators (LAMAs or LABAs) become standard. These keep your airways open for 12-24 hours. Pulmonary rehabilitation is strongly recommended. It’s not just exercise - it’s learning how to breathe efficiently, manage anxiety, and pace yourself. Studies show it cuts hospital visits by 37%. Vaccines remain essential. Many patients at this stage can still work, but may need to switch to less physically demanding roles.
Stage 3: Managing Flare-Ups
Combination inhalers - LAMA + LABA - are common. If you’ve had two or more flare-ups in a year, adding an inhaled corticosteroid (ICS) reduces hospitalizations. Oxygen therapy may be prescribed if your blood oxygen drops below 88% during activity or sleep. Nutrition matters too. Many with severe COPD lose weight because breathing burns so many calories. A dietitian can help.
Stage 4: Survival and Comfort
Continuous oxygen therapy (15+ hours daily) is life-extending. The NOTT study showed a 44% improvement in survival for those with severe low oxygen levels. Lung volume reduction surgery can help select patients by removing damaged lung tissue, giving healthier parts more room to work. Lung transplant is an option for those under 65 with FEV1 under 20% and no other major health issues. Palliative care becomes important - not just for end-of-life, but to manage symptoms, reduce anxiety, and improve daily function.

What Works Beyond Medication
Medicines help, but they’re only part of the picture. The most effective COPD management includes:
- Pulmonary rehabilitation: A structured program with exercise, education, and breathing training. Done right, it improves your daily life more than any drug.
- Vaccinations: Flu shot every year. Pneumococcal vaccine every 5-10 years. COVID-19 boosters as recommended. These prevent infections that can trigger deadly flare-ups.
- Nutrition: Eating enough protein and calories is hard when breathing takes so much energy. Small, frequent meals help.
- Home oxygen: For those with low blood oxygen, it’s not a luxury - it’s necessary for survival.
- Smoking cessation support: Even if you’ve smoked for 40 years, quitting at any stage helps. Nicotine patches, counseling, and medications like varenicline double your chances of success.
Many patients struggle with inhaler technique. Studies show 70-80% use them wrong. Ask your doctor or pharmacist to watch you use your inhaler - once, twice, even five times. Proper use makes all the difference.
Real People, Real Challenges
One man in his late 50s, diagnosed at Stage 2 after years of ignoring his cough, had to quit his warehouse job because he couldn’t walk 200 feet without stopping. Another woman in her 60s with Stage 4 says she can’t shower without her portable oxygen tank - and even brushing her teeth leaves her breathless.
But there are success stories too. A woman in her 70s started pulmonary rehab after her third hospitalization. Six months later, she was walking 20 minutes without stopping. Another man quit smoking at 68. His lung function didn’t bounce back, but his flare-ups dropped from four a year to one.
The biggest barrier? Cost. A single inhaler like Spiriva can cost $350-$400 a month without insurance. Portable oxygen units are heavy, bulky, and don’t last long on battery. Many patients feel trapped at home.
What’s New in COPD Treatment?
In 2023, the FDA approved Breztri Aerosphere, the first single-inhaler triple therapy for COPD. It combines three medications in one device - making it easier to take. Another new drug, ensifentrine, showed promise in trials, improving lung function by 13%.
Technology is helping too. The FDA-cleared Kyna COPD app tracks symptoms daily and uses AI to predict flare-ups 4-7 days in advance with 82% accuracy. That means you can call your doctor before you end up in the ER.
Research is also looking at genetics. The NIH’s COPDGene study found 82 genetic markers linked to how fast COPD progresses. In the future, treatment may be tailored to your DNA.
What You Can Do Today
If you’re over 40 and have smoked - even decades ago - and you’re short of breath, have a daily cough, or get tired easily, get tested. A simple spirometry test takes five minutes. It’s not painful. It doesn’t require needles.
If you’ve been diagnosed:
- Stop smoking - no exceptions.
- Take your meds exactly as prescribed.
- Learn how to use your inhaler - ask for a demonstration.
- Get vaccinated every year.
- Join a pulmonary rehab program if your doctor recommends it.
- Track your symptoms. Write down when you feel worse - what you did, how long it lasted, what helped.
- Don’t wait until you’re gasping to call your doctor. Early intervention prevents hospital stays.
COPD doesn’t have to mean giving up life. With the right care, many people live full, active years - even with Stage 3 or 4 disease. The goal isn’t just to breathe. It’s to live well while you do.
Can COPD be reversed?
No, COPD cannot be reversed. Once lung tissue is damaged, it doesn’t heal. But the progression can be slowed significantly - especially if you quit smoking early. Medications, pulmonary rehab, and oxygen therapy can help you maintain function and prevent complications. Many people with COPD live for decades with proper management.
Is COPD the same as asthma?
No. Asthma is usually reversible with medication and often starts in childhood. COPD is progressive, typically caused by smoking or long-term exposure to irritants, and usually starts after age 40. Some people have both - called asthma-COPD overlap syndrome (ACOS). Treatment for ACOS often includes a combination of asthma and COPD medications.
How do I know if I’m having a COPD flare-up?
Signs include increased shortness of breath, more frequent coughing, changes in mucus (more volume, thicker, or a different color like yellow or green), wheezing, fatigue, or swelling in your ankles. If you notice these, contact your doctor right away. Early treatment with antibiotics or steroids can prevent a hospital visit.
Do I need oxygen all the time?
Only if your blood oxygen levels are consistently low, usually below 88%. Your doctor will test this with a pulse oximeter or blood test. If you qualify, continuous oxygen (15+ hours a day) improves survival and reduces strain on your heart. You won’t need it all the time if your oxygen is normal at rest and during activity.
Can I still travel with COPD?
Yes, but it takes planning. Talk to your doctor before flying - cabin pressure is lower, which can lower your oxygen levels. You may need portable oxygen on the plane. Always carry extra medication, a copy of your prescription, and your doctor’s contact info. Avoid high altitudes and areas with heavy pollution. Many people with COPD travel successfully with the right preparation.
What’s the life expectancy with COPD?
It varies widely. Someone with mild COPD who quits smoking and follows treatment can live for many years - sometimes decades. Those with severe disease and frequent flare-ups may have a shorter life expectancy. But it’s not just about the stage - your overall health, activity level, and how well you manage the disease matter more than the number on a spirometry test. Many people live full lives well into their 80s with COPD.
Next Steps: What to Do Now
If you haven’t been tested and you’re at risk - get a spirometry test. It’s quick, affordable, and often covered by insurance. If you’ve been diagnosed, schedule a pulmonary rehab referral today. Ask your doctor about your inhaler technique. Review your vaccination status. Write down your symptoms and bring them to your next appointment.
COPD is serious, but it’s not a death sentence. The most powerful tool you have is knowledge - and action. Start today. Your lungs will thank you tomorrow.








Gillian Watson
December 5, 2025 AT 05:25Been living with Stage 3 for five years now. Pulmonary rehab saved my life. Not magic, just sweat and structure. I walk 3 miles most days now, oxygen tank on my back like a backpack. People stare, but I don’t care anymore.
Jessica Baydowicz
December 6, 2025 AT 01:58YESSSS! This is the most real, non-creepy medical post I’ve seen in years. 💪 I used to think COPD meant ‘couch potato disease’ until my aunt started rehab. Now she’s hiking in Colorado with her grandkids. Stop underestimating this stuff - it’s not a death sentence, it’s a lifestyle reset!
Benjamin Sedler
December 7, 2025 AT 20:34Wait - so you’re telling me smoking isn’t the only cause? What about those factory workers in Ohio breathing asbestos dust for 30 years? Or the guy who lived next to a coal plant? They didn’t light up once. But sure, let’s keep blaming the smokers. Classic.
Pavan Kankala
December 8, 2025 AT 03:26They’re lying. COPD is a scam. Big Pharma invented it to sell inhalers. Your lungs don’t ‘degrade’ - they’re just being poisoned by air ionizers, 5G towers, and fluoridated water. I’ve cured my cough with turmeric and a copper bracelet. Try it.
Ollie Newland
December 10, 2025 AT 01:14That Breztri Aerosphere? Game-changer. Triple combo in one device cuts down the inhaler chaos from six puffs to one. No more fumbling with three different devices when you’re wheezing. Also - inhaler technique? 80% of people use them wrong. Watch the video your pharmacist sends you. Seriously.
Martyn Stuart
December 11, 2025 AT 00:47For anyone reading this and thinking ‘I’m too old to quit’ - you’re not. My dad quit at 72 after 50 years of smoking. His FEV1 didn’t magically bounce back, but his flare-ups dropped from monthly to once a year. He’s still gardening. He’s still laughing. Age isn’t the enemy - apathy is.
Pulmonary rehab isn’t just for the young. My 78-year-old neighbor joined last year. Now she’s doing chair yoga with a group of women who all have COPD. They call themselves ‘The Oxygen Club.’ It’s beautiful.
And if cost is the barrier? Ask about patient assistance programs. Most pharma companies have them. You’d be shocked how many people don’t even know they exist.
Don’t wait until you’re gasping on the floor. Do one thing today. Call your doctor. Ask about spirometry. It’s five minutes. That’s all.
Rachel Bonaparte
December 11, 2025 AT 04:12Let’s be real - this whole ‘COPD is manageable’ narrative is just corporate wellness theater. You’re being sold a narrative that makes you feel like you’re in control, when in reality, you’re just a data point in a $200 billion pharmaceutical ecosystem. The real solution? Clean air. Universal healthcare. Ending industrial pollution. But no - we’d rather give you a $400 inhaler and call it a day. Meanwhile, the EPA ignores the fact that 1 in 3 Americans live in areas with unhealthy air. So yes - quit smoking. But also, demand systemic change. Or you’re just a cog in the machine.
And don’t get me started on the ‘Kyna COPD app.’ AI predicting flare-ups? That’s just surveillance capitalism with a stethoscope. They’re collecting your breathing patterns, your location, your medication adherence - and selling it to insurers. You think your data’s private? It’s not. You’re being monetized while you’re gasping for air.
And yes, I’ve read the NIH COPDGene study. 82 genetic markers? Fascinating. But who’s funding that? Big Pharma again. The real cure isn’t in your DNA - it’s in the air you breathe. And that’s being poisoned by the same corporations selling you the ‘solution’.
So yes - take your meds. Go to rehab. But don’t forget who really profits when you’re sick.
And if you think this post is ‘alarmist’ - ask yourself: why does the CDC say 14 million Americans have COPD, but estimates suggest 24 million are undiagnosed? Because the system doesn’t want you to know until it’s too late.
Carolyn Ford
December 13, 2025 AT 01:02Ugh. Another ‘COPD is manageable’ feel-good article. You people are so naive. You think quitting smoking fixes it? HA. I smoked for 30 years, quit at 55 - and still ended up on oxygen by 62. The damage was done. All these ‘success stories’? They’re outliers. The rest of us are just waiting for our last breath. And don’t even get me started on the cost of oxygen tanks - $1,200 a month? With insurance? Please. I’m on Medicaid and still pay $400 out of pocket. You call that ‘management’? It’s financial torture.
And don’t tell me to ‘get vaccinated.’ I’ve had five pneumonia shots. I’ve had the flu shot every year since 2008. And I still end up in the ER every winter. So don’t preach. Just… shut up.
Gareth Storer
December 14, 2025 AT 18:37So let me get this straight - you’re telling me that if I smoke for 40 years, then quit, I can ‘slow down’ the damage? Wow. What a revelation. Next you’ll tell me that if I drive drunk for 20 years, then stop, my liver won’t explode. Newsflash: some damage is permanent. You’re not ‘managing’ COPD - you’re just delaying the inevitable. And yes, I’m the guy who told you this in 2018. Still waiting for someone to listen.
jagdish kumar
December 16, 2025 AT 07:43Life is suffering. COPD is just one form of it. We are all breathing our last breaths, one molecule at a time. The air is poison. The world is decay. But still - we inhale. And that, perhaps, is the only true act of rebellion.
Yasmine Hajar
December 17, 2025 AT 16:43My mom had Stage 4. She used to say, ‘I’m not dying of COPD - I’m living with it.’ She’d sit on the porch with her oxygen tank, sip tea, and watch the birds. She didn’t let it take her spirit. And she lived to 84. That’s the real story. Not the numbers. Not the inhalers. The will to keep seeing sunrises.
To anyone scared: you’re not alone. We’ve all been there. But you can still laugh. You can still hug. You can still live. Just… take it slow.
Michael Feldstein
December 17, 2025 AT 17:03Just wanted to add - if you’re using a spacer with your inhaler, you’re doing it right. Most people don’t. And if you’re not? Go to YouTube and search ‘inhaler technique with spacer.’ Watch the video. Do it in front of a mirror. Do it three times. It’s the single biggest upgrade you can make to your treatment. Seriously. I’ve seen people go from needing ER visits every month to none in six months just by fixing their technique.
Also - if you’re using a rescue inhaler more than twice a week? That’s your body screaming for help. Don’t wait. Call your doctor. Today.