Drug Risk Calculator
Calculate Your Risk
Personalized Risk Assessment
Key Interactions Detected:
When you take a medication, you expect it to help - not hurt. But if you have one or more chronic health conditions, the risk of bad reactions doesn’t just go up a little. It skyrockets. A person with multiple health problems is nearly three times more likely to suffer an adverse drug reaction than someone who’s otherwise healthy. That’s not a small risk. It’s a life-altering one.
Why Existing Conditions Make Drugs More Dangerous
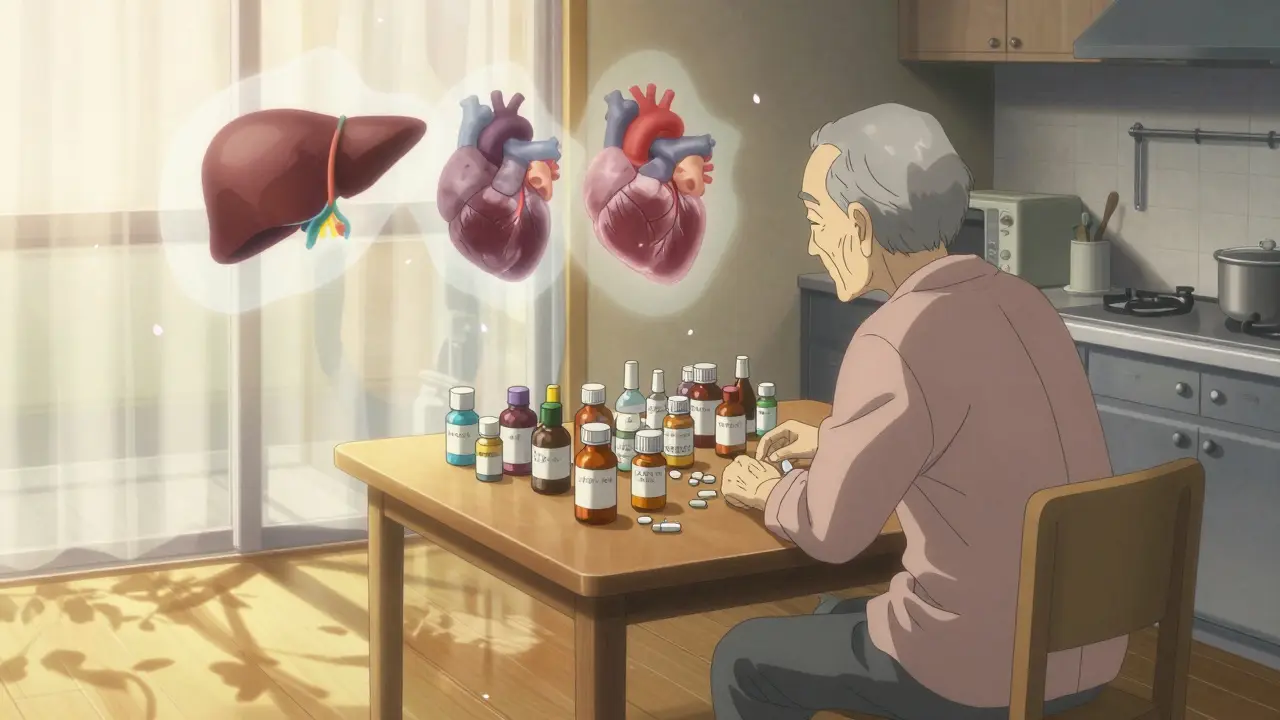
Your body doesn’t treat every drug the same way. When you have liver disease, kidney problems, heart failure, or diabetes, your body’s ability to process medicine changes. These aren’t just minor tweaks - they’re major shifts in how drugs move through your system. Take liver disease, for example. The liver uses enzymes - especially the CYP450 family - to break down most medications. When the liver is damaged, those enzymes drop by 30% to 50%. That means drugs like painkillers, antidepressants, or blood thinners stay in your body longer. Instead of being cleared safely, they build up. And that buildup can cause dizziness, confusion, bleeding, or even organ failure. Kidney problems do something similar. If your kidneys can’t filter waste properly, drugs that are cleared through urine - like certain antibiotics, diuretics, or diabetes meds - stick around too long. Even a 30% drop in kidney function can turn a safe dose into a toxic one. It’s not just about how your body handles the drug. Your diseases also make you more sensitive to the drug’s effects. Someone with Parkinson’s might react violently to an antipsychotic that’s fine for others. Someone with heart failure might crash from a blood pressure pill that’s perfectly safe for a healthy person. This is called a pharmacodynamic interaction - your disease changes how your body responds to the medicine.The Polypharmacy Trap
Most people with multiple chronic conditions don’t take just one drug. They take five, seven, or even ten. In Australia, nearly half of adults over 65 with three or more conditions are on five or more medications daily. That’s called polypharmacy. And it’s where the real danger lies. Each new drug adds another layer of risk. Not just because of the drug itself, but because of how it interacts with the others. One study found that 47% of elderly patients on multiple drugs had at least one dangerous interaction. Over a third of those were major - meaning they could cause permanent harm or death. Cancer patients are especially vulnerable. In one group of 100 cancer patients, researchers found 65 separate drug-drug interactions. More than one-third were classified as major. That’s not rare. That’s routine. And here’s the catch: many of these drugs were prescribed by different doctors. One prescribes the blood thinner. Another prescribes the painkiller. A third adds an antidepressant. No one sees the full picture. And no one checks how they all work together.Who’s Most at Risk?
It’s not just older adults. Though they’re the most common group affected, anyone with multiple chronic conditions is at risk. Here are the top comorbidities that turn routine drugs into potential hazards:- Heart disease + blood thinners = higher bleeding risk
- Diabetes + certain antibiotics = dangerous blood sugar swings
- Liver disease + pain meds or sedatives = overdose risk
- Kidney disease + NSAIDs or diuretics = acute kidney injury
- Depression or anxiety + opioids or benzodiazepines = respiratory depression
- Chronic pain + opioids = addiction risk and overdose

What Symptoms Should You Watch For?
Side effects in people with comorbidities don’t always look like typical drug reactions. They’re often subtle - and easily mistaken for the disease getting worse. The most common signs in patients with multiple conditions:- Weakness or fatigue (36% of cases)
- Dizziness or lightheadedness (12%)
- Headaches (7%)
- Nausea or vomiting (5%)
- Insomnia or confusion (3%)
Why Doctors Miss These Risks
You’d think doctors would know this. But here’s the truth: most clinical trials exclude people with multiple chronic conditions. In fact, 70% to 80% of elderly patients with comorbidities are left out of drug studies. That means the dosing instructions on the label were never tested on the people who need them most. Add to that: most doctors see patients for 10 to 15 minutes. They’re not trained to track every drug, every condition, every interaction. And when you’re seeing five different specialists, each focused on one organ or disease, no one is looking at the whole picture. A 2025 study found that 45.7% of older patients were prescribed at least one medication listed as potentially inappropriate for their age and conditions. That’s nearly half. And women over 75 were nearly three times more likely to get these risky drugs than younger patients.
What Can You Do?
You don’t have to accept this risk. There are steps you can take right now.- Get a full medication review. Ask your GP or a clinical pharmacist to sit down with you and go over every pill, patch, and injection you take - including over-the-counter drugs and supplements. This alone has been shown to reduce side effects by 22%.
- Use one pharmacy. If you fill prescriptions at multiple places, no one sees the full list. One pharmacy can flag dangerous interactions.
- Keep a written list. Include the name, dose, reason, and who prescribed it. Bring it to every appointment.
- Ask: “Could this interact with my other conditions?” Don’t just accept a new prescription. Ask if it’s safe given your heart, liver, or kidney health.
- Check for deprescribing. Sometimes, the safest choice is to stop a drug. Tools like STOPP/START help doctors identify which meds can be safely reduced or removed.
The Future Is Personalized
The good news? Things are changing. In 2024, the NIH launched a new database that tracks 12 million patient records to find dangerous drug-comorbidity pairs. They’ve already found 217 new high-risk combinations. Machine learning tools now predict adverse reactions with 89% accuracy - far better than old methods. And new tools like the American Medical Association’s 2025 Comorbidity Assessment Tool adjust risk scores in real time using your latest lab results. Soon, doctors may use your genetic profile, organ function, and disease history to build a custom drug plan - one that’s not based on averages, but on you. Until then, the safest thing you can do is stay informed. Know your conditions. Know your meds. Ask the hard questions. Because when it comes to drugs and comorbidities, the difference between safety and disaster isn’t luck. It’s awareness.Can one chronic condition make a drug dangerous even without other medications?
Yes. Even a single chronic condition like liver disease, kidney failure, or heart failure can change how your body handles a drug. For example, liver disease reduces the enzymes that break down medications, causing them to build up to toxic levels. A standard dose of a painkiller or antidepressant could become dangerous - even if you’re not taking any other drugs.
Are over-the-counter drugs and supplements safe if I have comorbidities?
Not necessarily. Many people assume OTC meds are harmless, but that’s not true. Ibuprofen can harm kidneys in people with heart or kidney disease. St. John’s Wort can interfere with blood thinners and antidepressants. Even common antacids can affect how other drugs are absorbed. Always check with a pharmacist before taking anything new.
Why don’t doctors always warn me about these risks?
Many doctors aren’t trained to manage complex polypharmacy. Clinical trials rarely include patients with multiple conditions, so drug labels don’t reflect real-world risks. Plus, with short appointment times and fragmented care, it’s easy for interactions to be missed. That’s why it’s critical for you to ask questions and keep your own records.
Can I reduce my risk by stopping some of my medications?
Sometimes, yes. Many older adults are on medications that were prescribed years ago and are no longer needed - or are doing more harm than good. Tools like STOPP/START help doctors identify which drugs can be safely stopped. Never stop a medication on your own, but do ask your doctor if any of your prescriptions can be reduced or removed.
How do I know if a side effect is from a drug or my disease getting worse?
It’s often hard to tell. Weakness, dizziness, confusion, and nausea can be signs of either. But if these symptoms started after a new drug was added - or changed in dose - it’s likely drug-related. Track when symptoms began and share that timeline with your doctor. A simple rule: if it started after a new pill, suspect the pill.
Is this problem getting worse?
Yes. By 2030, 90% of adults over 65 will have two or more chronic conditions. At the same time, drug use is rising. That means more people are at risk. But awareness is also growing. New tools, databases, and AI systems are being developed to help catch these risks before they cause harm.






Gran Badshah
December 28, 2025 AT 16:07Man, I saw this with my dad-he had liver cirrhosis and was on like 7 meds. One day he just passed out after taking his painkiller. No warning. No one told him the dose was toxic for his liver. They just kept prescribing like he was a healthy 30-year-old. Scary as hell.
Ellen-Cathryn Nash
December 30, 2025 AT 00:26It’s not just about drugs-it’s about the entire medical industrial complex being built on the backs of vulnerable people. They test meds on young, healthy men, then sell them to grandmas with 5 chronic conditions and call it ‘evidence-based.’ It’s not science. It’s profit-driven negligence.
Debra Cagwin
December 31, 2025 AT 02:40If you or a loved one is managing multiple conditions, please-do not wait for a crisis. Request a full med review with a clinical pharmacist. It’s free in most hospitals, takes less than an hour, and can literally save your life. I’ve seen it turn confusion into clarity, fatigue into energy. You’re not being a burden-you’re being proactive. And that’s powerful.
Hakim Bachiri
December 31, 2025 AT 10:14Celia McTighe
December 31, 2025 AT 20:42My grandma took a new blood pressure med and started walking into walls. We thought it was dementia. Turns out, it was the drug + her kidney function dropping. She got her meds reviewed, two were pulled, and she’s been walking fine for 8 months now. 🙏 Please, if you’re on more than 5 meds, get a review. You’re not being paranoid-you’re being smart.
Ryan Touhill
January 1, 2026 AT 00:44Let’s be honest-this is the inevitable outcome of a system that treats the human body like a machine with interchangeable parts. Doctors are trained to fix one organ, not to see the whole organism. And when you layer on polypharmacy, you’re not treating disease-you’re conducting a biochemical experiment on a living person. And the worst part? They don’t even tell you.
Teresa Marzo Lostalé
January 2, 2026 AT 05:55You know what’s wild? The same people who say 'trust the science' are the ones who ignore that 80% of clinical trials exclude people like us. So the science they're trusting? It doesn’t even apply to the people who need it most. We’re living in a world where the data is broken, but the prescriptions keep coming.
ANA MARIE VALENZUELA
January 2, 2026 AT 17:24Stop acting like this is new. People have been dying from bad drug combos since the 1970s. The only thing that’s changed is the marketing. Now they slap ‘personalized medicine’ on it and act like it’s a breakthrough. It’s not. It’s damage control. And your ‘tools’? They’re still in beta. Don’t let corporate jargon fool you.
Bradly Draper
January 3, 2026 AT 10:30I didn’t know any of this until my mom had a stroke after taking a new antibiotic. She had kidney issues. The doc didn’t ask about her meds. Just said, ‘It’s fine.’ She’s okay now, but I’ll never forget how scared I was. Just ask questions. Even if it feels dumb.
Samantha Hobbs
January 3, 2026 AT 11:17My aunt took St. John’s Wort with her blood thinner and almost bled out. She thought it was ‘natural’ so it was safe. NO. IT’S NOT. Just because it’s in a bottle at the grocery store doesn’t mean it’s not poison with your conditions. Talk to a pharmacist. Not your cousin who ‘reads a lot on Reddit.’
Nicole Beasley
January 4, 2026 AT 20:31OMG I just realized my dad’s fatigue is probably from his meds, not ‘just getting older’ 😳 I’m scheduling a med review this week. Thank you for this post!! 🙌❤️
sonam gupta
January 6, 2026 AT 01:07Julius Hader
January 7, 2026 AT 05:04It’s not the drugs. It’s the lack of accountability. If a car company sold a vehicle that killed 47% of its customers under normal use, they’d be in prison. But doctors? They get awards. And pharmaceuticals? They get tax breaks. This isn’t medicine. It’s a moral failure.
Vu L
January 7, 2026 AT 12:50Wait, so you’re telling me the system is broken? Shocking. I thought the FDA was all-powerful. Turns out, they’re just glorified paper-pushers who approve stuff because the company paid for the study. Who knew? 😂
James Hilton
January 9, 2026 AT 04:35Just got off the phone with my pharmacist. She pulled 3 meds I didn’t even know were dangerous with my heart condition. One was a supplement I’d been taking for 12 years. I felt like a fool. But now? I feel alive. Ask. Review. Listen. Your life isn’t a gamble.