What Is TENS Therapy?
TENS therapy is a non-drug pain relief method that uses low-voltage electrical pulses delivered through electrodes on the skin to interfere with pain signals before they reach the brain. It stands for Transcutaneous Electrical Nerve Stimulation, and it’s been used for over 50 years to help people manage both acute and chronic pain without pills or injections.
Unlike medications that change how your body chemistry works, TENS works by sending gentle electrical signals through your skin to your nerves. These signals can either block pain messages from getting through or trigger your body’s natural painkillers-chemicals called endorphins. It’s not a cure, but for many people, it’s a reliable way to reduce pain when used correctly.
How TENS Actually Stops Pain
There are two main ways TENS reduces pain, and the settings on your device determine which one kicks in.
The first is called the gate control theory. This idea, first proposed in 1965, says your spinal cord has a kind of gate that controls whether pain signals get sent to your brain. When you use TENS at a high frequency (50-100 Hz), it activates large, fast-moving nerve fibers that carry touch and vibration signals. These signals flood the gate, making it harder for slower, painful signals to get through. Think of it like turning up the volume on music to drown out a shout. You still feel the tingling from the device, but your pain fades.
The second way is through your body’s own painkillers. When you set your TENS unit to low frequency (2-5 Hz) and crank up the intensity, it stimulates different nerves that signal your brain to release endorphins. These are the same chemicals your body makes during exercise or after a good laugh. This effect takes longer to kick in-usually 20-30 minutes-but the pain relief can last for hours after you turn the device off.
Some modern TENS machines have a burst mode that mixes both approaches: short bursts of high-frequency pulses followed by pauses. This gives you the immediate blocking effect plus the endorphin boost. It’s often the most effective setting for people with long-term pain.
Who Benefits Most From TENS?
TENS isn’t a magic wand, but it works well for certain types of pain.
For acute pain-like after surgery, a sprained ankle, or during labor-TENS can cut pain by 30% or more. A 2020 Cochrane Review found women using TENS during childbirth reported significantly less pain than those using placebo devices.
For chronic pain, results are mixed but promising for specific conditions:
- Osteoarthritis: Studies show 35% more pain reduction than placebo, especially in knees and hands.
- Lower back pain: Works better than sham devices, but not as well as physical therapy or movement-based treatments.
- Neuropathic pain: Some people with diabetic nerve pain or sciatica report major relief, especially when electrodes are placed along the nerve pathway.
- Fibromyalgia: Only about 38% of users get meaningful relief, so it’s not a go-to for this condition.
People who avoid opioids or can’t tolerate their side effects (like drowsiness, nausea, or constipation) often turn to TENS. One study showed TENS users cut their opioid use by nearly 27% after surgery.
What You Need to Know About Settings
Most TENS units let you adjust three things: frequency (Hz), pulse width (microseconds), and intensity (mA). Getting these right makes the difference between a useless tingle and real relief.
High-frequency TENS (50-100 Hz): Best for sharp, sudden pain. Use low to medium intensity. You should feel a strong tingling or buzzing, but never pain. This is the go-to for post-surgery pain or muscle spasms.
Low-frequency TENS (2-5 Hz): For dull, aching, long-term pain. Use higher intensity-enough to feel a strong tapping or pulsing sensation. This triggers endorphins. It takes longer to work, so use it for 20-30 minutes at a time.
Burst mode: A hybrid. Sets deliver pulses in groups of 3-5 high-frequency bursts per second. Good for mixed pain types. Many modern units have preset programs labeled “acute,” “chronic,” or “burst.”
Intensity: This is where most people fail. A 2009 study found 68% of failed TENS treatments happened because the user didn’t turn the intensity up high enough. If you can barely feel it, it won’t work. Aim for a strong but comfortable sensation. You should never feel sharp pain or muscle cramping.
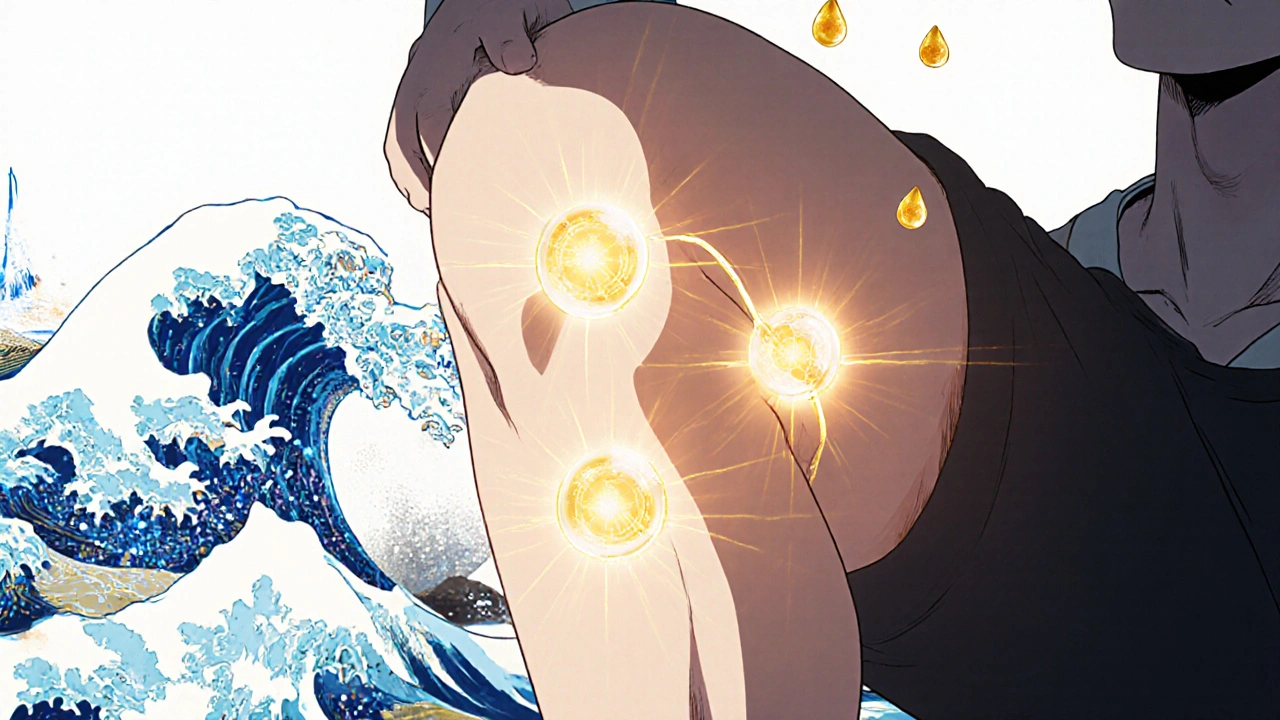
Where to Place the Electrodes
Electrode placement is everything. Put them in the wrong spot, and you’ll get zero relief.
For localized pain-like a sore knee or lower back-place electrodes directly over or within 1-2 inches of the painful area. If your pain runs along a nerve (like sciatica), place electrodes along the nerve’s path, not just at the end point.
Common placements:
- Lower back pain: One pair above the hips, one below the rib cage.
- Knee pain: One on each side of the kneecap.
- Neck pain: Behind the ears and down the upper trapezius muscles.
- Shoulder pain: On the deltoid and upper arm.
Never place electrodes over broken skin, open wounds, or directly on the front of your neck, eyes, or chest if you have a pacemaker. Two electrodes should never cross the heart. Always follow the diagram in your manual.
Pro tip: Use conductive gel if your electrodes start slipping or losing signal. It cuts resistance by over 60%, making your treatment more consistent.
Real User Experiences
People’s stories about TENS vary wildly-and that’s normal.
On Amazon, 78% of users who gave positive reviews said they felt relief while using the device. One user wrote: “I had a flare-up of sciatica. Put the pads on my lower back and hip. Within 10 minutes, I could stand up straight. Didn’t need my painkillers that day.”
But others say it doesn’t work. A Reddit user shared: “I tried it for 6 months. It tickles. That’s it. I don’t know if I’m doing it wrong or if it just doesn’t work for me.”
Why the difference? Most often, it’s intensity or placement. One study of 342 patients found 41% of failures were due to electrodes being placed too far from the pain source. Another common issue: battery life. At high intensity, most units last 8-10 hours. If you’re using it all day, you’ll need spare batteries or a rechargeable model.
Side effects are rare, but 34% of users report skin irritation from the adhesive pads. Switching brands or using hypoallergenic electrodes helps. Some people also feel muscle twitching-this is normal if you’re using low-frequency mode.
What’s New in TENS Technology
TENS isn’t stuck in the 1980s. The market is evolving fast.
In May 2023, the FDA cleared the first AI-powered TENS device, NeuroLoop AI. It uses sensors to read your body’s response in real time and adjusts the settings automatically. In a trial, it delivered 44% more pain relief than traditional units.
Companies are also building “smart electrodes” with tiny sensors that monitor skin resistance. If your sweat makes the connection weak, the device boosts the current to keep the signal steady. The NIH just funded $2.4 million to bring these to market.
Many new units connect to apps via Bluetooth. You can track your usage, save your best settings, and even get guided sessions. This is a big help for beginners who don’t know how to adjust settings.
On the business side, TENS is growing. The global market hit $498 million in 2022 and is expected to top $780 million by 2028. In the U.S., Medicare reimburses $150 for a TENS unit if prescribed for chronic pain. Companies like Amazon now offer TENS devices in workplace wellness programs to cut down on injury-related absences.
When TENS Won’t Help-and When to Stop
TENS isn’t for everyone.
Don’t use it if you:
- Have a pacemaker or implanted defibrillator
- Are pregnant (unless under medical supervision for labor)
- Have cancer in the area you want to treat
- Have broken or irritated skin where the pads go
- Have epilepsy and are placing electrodes near your head or neck
Also, if you’re on opioid medications, low-frequency TENS might not work as well. Research shows opioids can block the endorphin response, making the body’s natural painkillers less effective.
And if you’ve tried TENS properly for 2-4 weeks with no improvement, it’s probably not for you. There’s no harm in stopping. It’s not addictive, and you haven’t wasted time-you’ve learned what doesn’t work.
How to Get Started
You don’t need a prescription to buy a TENS unit. They’re sold online, in pharmacies, and medical supply stores. Prices range from $30 for basic models to $300 for professional-grade units with smart features.
Start with a reputable brand like Omron, TechCare, or Chattanooga. Look for units with:
- At least two channels (so you can use four electrodes)
- Adjustable frequency and intensity
- Pre-set programs for back, knee, or neck pain
- Rechargeable battery or easy battery replacement
Before you use it, watch a video from a physical therapist or read the manual cover to cover. Many people skip this and get frustrated. If you can, ask your physiotherapist to show you how to place the pads and set the right intensity. Even one 20-minute session can save you weeks of trial and error.
Use it for 20-40 minutes at a time, up to three times a day. Don’t leave it on while sleeping. Keep a log: note your pain level before and after, how long you used it, and what settings worked. After a week, you’ll know if it’s worth sticking with.
Final Thoughts
TENS therapy isn’t a miracle cure. But for millions of people with back pain, arthritis, or nerve pain, it’s a tool that actually works-when used right. It’s safe, drug-free, and portable. You can use it at your desk, in the car, or while watching TV.
The biggest mistake? Underusing it. Turn the intensity up. Move the pads closer to the pain. Try a different setting. Don’t give up after one try. And if you’re unsure, talk to a physical therapist. They’ve seen what works and what doesn’t.
In a world where pain meds come with risks, TENS offers a quiet, powerful alternative. It doesn’t fix the cause of your pain-but sometimes, just taking the edge off is enough to get your life back.
Can I use TENS every day?
Yes, most people use TENS daily for chronic pain, typically 2-4 times a day for 20-40 minutes per session. There’s no evidence that daily use causes harm, as long as you follow safety guidelines and avoid using it on broken skin or over sensitive areas. If your skin becomes irritated, take a day off and switch to hypoallergenic electrodes.
Does TENS help with nerve pain?
Yes, especially for nerve-related pain like sciatica, diabetic neuropathy, or post-herpetic neuralgia. The key is placing electrodes along the path of the affected nerve-not just at the point of pain. Low-frequency or burst mode settings often work best for nerve pain because they stimulate endorphin release and block abnormal nerve signals.
How long does TENS pain relief last?
It depends on the mode. High-frequency TENS usually only works while you’re using it. Low-frequency or burst mode can provide relief that lasts 1-6 hours after turning it off. Some users report effects lasting up to 24 hours after multiple sessions, especially with consistent daily use. The longer-term benefit comes from training your nervous system to respond better to pain signals over time.
Is TENS covered by insurance?
In the U.S., Medicare and some private insurers cover TENS units under code E0720 if prescribed for chronic pain. You’ll need a doctor’s note and proof that other treatments failed. Coverage varies by plan. In Australia, TENS is not covered by Medicare, but some private health funds offer rebates under ancillary benefits. Always check with your provider before buying.
Can I use TENS with other pain treatments?
Absolutely. TENS works well alongside physical therapy, stretching, heat therapy, and even low-dose pain medications. It’s often part of a multimodal approach. The CDC recommends non-drug therapies like TENS as a first step for chronic pain, especially to reduce reliance on opioids. Just avoid using it at the same time as other electrical devices like muscle stimulators unless directed by a professional.
Why does TENS sometimes stop working?
Your body can adapt to the electrical stimulation over time, especially if you use the same settings daily. This is called tolerance. To reset it, change your electrode placement, switch modes (e.g., from high to low frequency), or take a break for a few days. Also, check your electrodes-they lose stickiness after 5-10 uses. Replace them if they’re worn out or not adhering well.






Don Angel
November 19, 2025 AT 17:15benedict nwokedi
November 19, 2025 AT 20:02deepak kumar
November 19, 2025 AT 21:06Dave Pritchard
November 21, 2025 AT 13:09kim pu
November 21, 2025 AT 16:13malik recoba
November 22, 2025 AT 18:27Sarbjit Singh
November 23, 2025 AT 15:38Angela J
November 24, 2025 AT 00:18Sameer Tawde
November 25, 2025 AT 10:58Jeff Hakojarvi
November 26, 2025 AT 04:07Timothy Uchechukwu
November 27, 2025 AT 11:35Ancel Fortuin
November 28, 2025 AT 21:19Hannah Blower
November 30, 2025 AT 11:25Gregory Gonzalez
December 1, 2025 AT 20:25Ronald Stenger
December 2, 2025 AT 06:25