Polypharmacy: Risks, Interactions, and How to Stay Safe with Multiple Medications
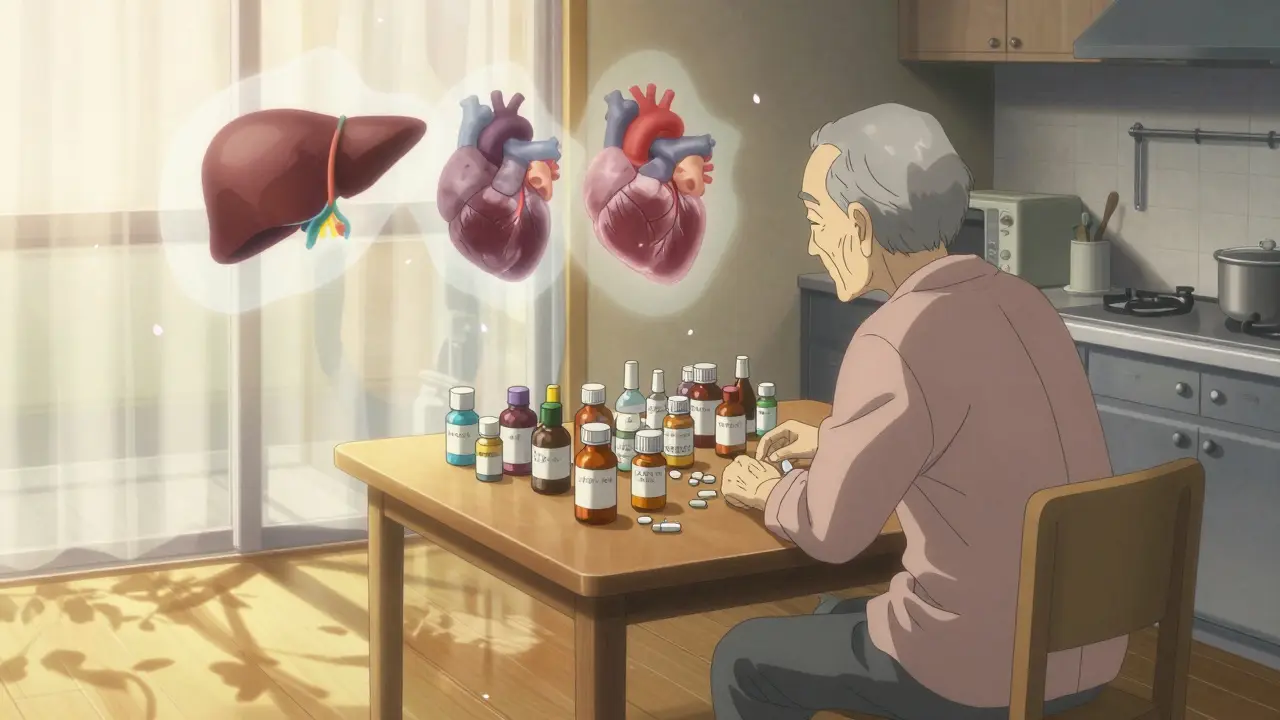
When you’re taking polypharmacy, the use of multiple medications by a single patient, often for different conditions. Also known as multiple drug therapy, it’s not just a medical term—it’s a daily reality for millions of older adults and people managing chronic illnesses. It’s not the number of pills that’s the problem—it’s what happens when those pills talk to each other. Some combinations can drop your blood sugar too low, spike your blood pressure, or leave you dizzy and confused. And if you’re not tracking them, you won’t even know it’s happening until something goes wrong.
Think of your body like a busy intersection. Every drug you take is a car entering that intersection. Add too many, and the traffic jams up. drug interactions, when two or more medications affect each other’s action in the body are the crashes. A diabetes drug like metformin might work fine alone, but throw in a common antibiotic, and your kidneys struggle. Or take a blood pressure pill like valsartan with a decongestant spray, and your pressure could shoot up. These aren’t rare accidents—they happen every day in homes, nursing facilities, and clinics. And they’re often missed because doctors focus on one condition at a time, not the whole pile of pills.
medication safety, the practice of ensuring drugs are used correctly to avoid harm isn’t just about taking them on time. It’s about knowing what’s in your medicine cabinet and why. Smart pill dispensers help track doses, but they don’t tell you if your lisinopril is reacting with your ibuprofen. Rebound nasal congestion from overused sprays? That’s a classic side effect of poor polypharmacy management. Even something as simple as alcohol can turn a safe dose of Mirabegron into a heart risk. The real danger isn’t the drugs themselves—it’s the lack of a full picture.
And it’s not just seniors. People with diabetes, autoimmune diseases like scleroderma, or chronic pain often juggle five, six, even ten prescriptions. Some take DPP-4 inhibitors for blood sugar, beta-blockers for heart rate, and antihistamines for allergies—all without realizing how they stack up. One wrong combo can mean hospital visits, falls, or organ damage. That’s why checking for interactions isn’t optional—it’s survival.
You don’t need to be a pharmacist to protect yourself. Start by keeping a real list—names, doses, why you take them. Bring it to every appointment. Ask your doctor: "Is this still necessary?" and "Could this interact with anything else I’m taking?" You’d be surprised how often a pill can be dropped, switched, or replaced with a non-drug option like TENS therapy for pain. And if you’re on more than five medications, consider a medication review. It’s not a luxury—it’s a standard of care.
Below, you’ll find real stories and practical guides on how polypharmacy affects everything from workplace safety to kidney function, from forgotten doses to dangerous overlaps between diabetes meds, antibiotics, and blood pressure drugs. These aren’t theory pieces—they’re lessons from people who’ve been there. Whether you’re managing your own meds or helping a loved one, this collection gives you the tools to cut through the noise and take back control.
How Comorbidities Increase Drug Side Effects and Risk
Comorbidities like liver disease, kidney failure, or heart conditions dramatically increase the risk of dangerous drug side effects. Learn how chronic illnesses change how your body processes medication - and what you can do to stay safe.
Brown Bag Medication Review Events: How to Prepare for a Safe and Accurate Medication Checkup
Learn how a brown bag medication review can prevent dangerous drug interactions, reduce unnecessary pills, and improve safety for anyone taking multiple medications. A simple, proven practice that saves lives.