Pharmacokinetic Tolerance: What It Is and How It Affects Your Medications
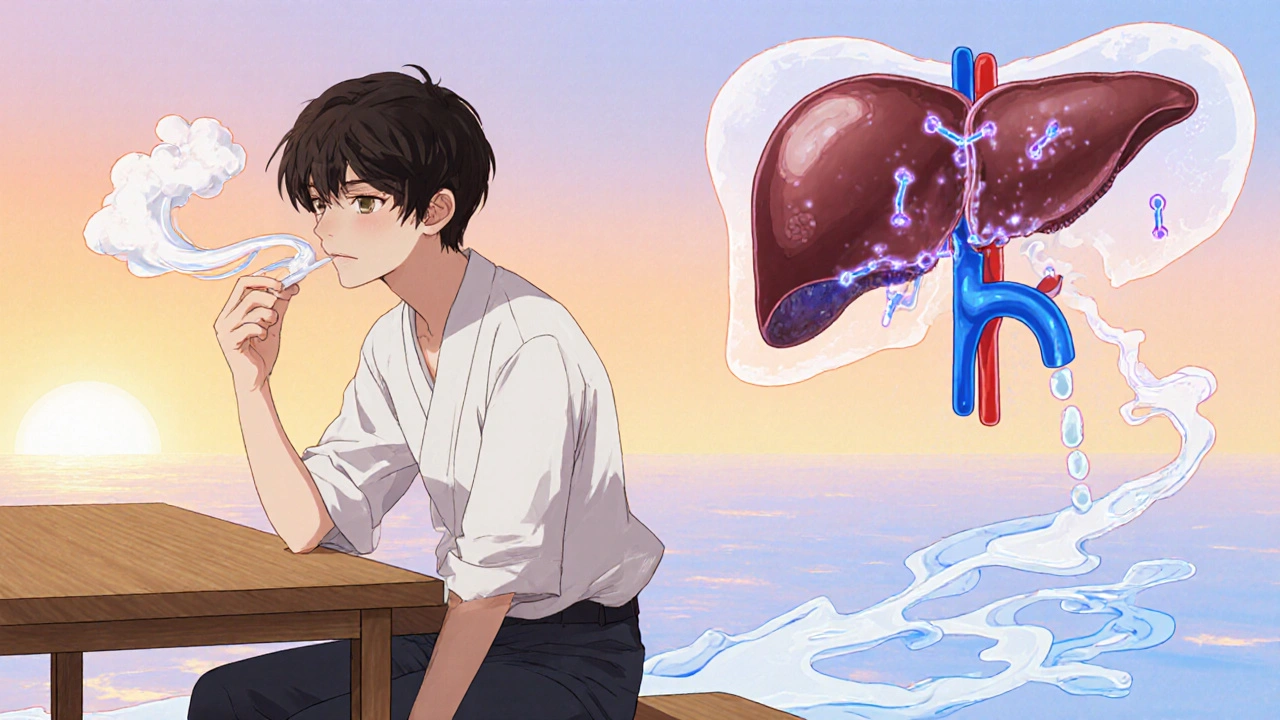
When your body starts to handle a drug differently over time, making it less effective, you’re likely dealing with pharmacokinetic tolerance, a change in how your body absorbs, distributes, metabolizes, or eliminates a drug. Also known as metabolic tolerance, it’s not about your brain getting used to the drug—it’s about your liver, kidneys, and enzymes working faster to clear it out. This is why some people need higher doses of painkillers, blood pressure meds, or even antibiotics after weeks or months of use. It’s not addiction. It’s biology.
Pharmacokinetic tolerance happens when your body increases the production of enzymes—like those in the CYP450 family—that break down medications. For example, if you take a drug regularly, your liver may start producing more of the enzyme that metabolizes it, so the drug leaves your system quicker. That means less of it stays in your bloodstream to do its job. This is different from pharmacodynamic tolerance, where the body’s response to the drug weakens at the cellular level. One is about how fast the drug is cleared; the other is about how well your cells respond to it.
It shows up in real life. Someone on long-term clarithromycin, an antibiotic used for infections, might find it stops working as well after a few weeks—not because the bacteria are resistant, but because their body is clearing it too fast. The same thing can happen with valsartan, a blood pressure medication, or even sertraline, an antidepressant. Your body doesn’t ignore the drug—it just gets better at removing it.
Not all drugs cause this. Some stay steady in your system no matter how long you take them. But for others, especially those processed by the liver, pharmacokinetic tolerance can quietly reduce their power. That’s why doctors sometimes switch meds, adjust dosing, or add enzyme inhibitors to slow down clearance. It’s also why you shouldn’t increase your dose on your own—what feels like "needing more" might just be your body adapting.
What you’ll find in the posts below are real-world examples of how this plays out. From how pharmacokinetic tolerance affects antibiotic use to why certain blood pressure drugs lose punch over time, these articles break down the science without the jargon. You’ll see how it connects to common medications like mirabegron, bicalutamide, and alendronate—not because they all cause tolerance, but because understanding how your body handles drugs helps you make smarter choices with any treatment.
Why Medication Side Effects Fade: Understanding Tolerance Development
Learn why certain medication side effects fade over time, the mechanisms behind drug tolerance, and how clinicians manage differential tolerance for better outcomes.