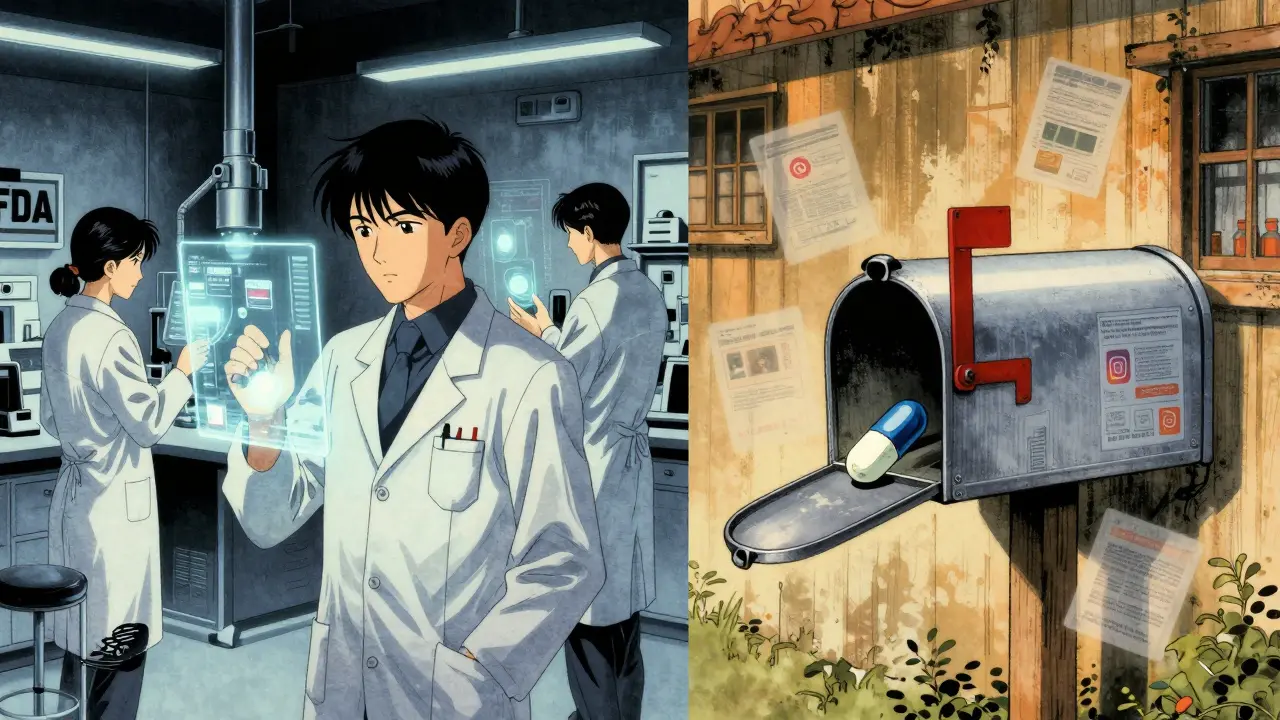
How the FDA Stops Unsafe Drugs Before They Reach U.S. Shelves
Every year, over 100 million drug shipments enter the United States. Most come from overseas manufacturers in countries like India, China, Germany, and Ireland. The FDA doesn’t inspect every single one. In fact, it physically examines less than 1.2% of them. So how does it stop dangerous, fake, or contaminated drugs from reaching pharmacies and hospitals? The answer isn’t luck-it’s a highly targeted, data-driven system built on risk, rules, and real-time alerts.
The FDA’s import inspection system isn’t just about checking boxes. It’s a living, evolving defense line against counterfeit painkillers, tainted antibiotics, and unapproved cancer drugs. Since 2023, there’s been a major shift: all FDA-regulated drug shipments, no matter how small or cheap, are now subject to review. That means even a $50 package of pills shipped directly to a consumer’s home gets flagged. This change came after years of abuse-illicit pill presses, fentanyl-laced capsules, and unregulated weight-loss drugs slipping through old loopholes.
The Five-Step FDA Import Process
The FDA doesn’t wait for drugs to hit the dock. It starts reviewing them before they even leave the port abroad. Here’s how it works:
- Entry Submission - Importers must file electronic notices through the FDA’s Prior Notice System Interface (PNSI). This includes product details, manufacturer info, shipping route, and certification that the product meets U.S. standards. Missing or wrong info? The shipment gets flagged immediately.
- Entry Review - A risk-based algorithm scans every submission. It looks at the manufacturer’s history, past violations, product type, country of origin, and even the importer’s track record. About 98% of entries are screened this way. If something raises a red flag-say, a company with a history of FDA warnings-the system auto-prioritizes it for inspection.
- Examination and Sampling - If flagged, the shipment is held at the port. FDA inspectors might do a physical check of the packaging, verify labels match FDA requirements, or take samples for lab testing. A single shipment can get 1 to 3 units pulled for analysis. Labs test for potency, contaminants, and whether the drug even contains what’s listed on the label.
- Compliance Review - Inspectors cross-check everything against U.S. law: Is the facility registered? Is the product approved? Are the labels in English? Is it following current good manufacturing practices (cGMP)? If any of these fail, the product gets detained.
- Final Admissibility Decision - The FDA either releases the shipment or refuses it. In 2022, 14.3% of physically examined drug shipments were detained. Of those, nearly 68% were permanently blocked from entering the U.S.
Who Gets Special Treatment? The SSCPP Program
Not all manufacturers are treated the same. The FDA runs a program called the Secure Supply Chain Pilot Program (SSCPP), launched in 2019. It’s designed for companies with a perfect compliance record. If a manufacturer has passed three straight years of clean inspections, they can apply to join. Once approved, up to five of their products get fast-tracked through U.S. ports.
For companies like Johnson & Johnson, this means clearance times drop from 7-10 days to under 48 hours. It’s a huge advantage for just-in-time manufacturing and supply chain reliability. But here’s the catch: only 27 companies were in the program as of late 2023. Most are big-name pharma players. Smaller generic drug makers, especially those sourcing active ingredients from India or China, rarely qualify. And even if they do, the application process is intense-requiring internal audits, documentation trails, and constant monitoring.
Why Some Ports Are Much Tougher Than Others
The FDA doesn’t have inspectors at every U.S. port. But Customs and Border Protection (CBP) does. So the pressure isn’t evenly distributed. At the Port of Los Angeles, only 5.2% of drug shipments were detained in 2022. At the Port of Miami? That number jumped to 18.7%. Why? It’s not random. Miami handles more shipments from Latin America and the Caribbean, where regulatory oversight is weaker. Los Angeles gets more from Asia, where many manufacturers have long-standing FDA relationships.
Also, some ports have dedicated FDA teams with deep knowledge of specific product types. If you’re shipping insulin from Germany, you’ll want your shipment routed through a port where inspectors have handled insulin before. Experienced importers know this. They build relationships with specific FDA entry reviewers-sometimes even scheduling pre-submission calls. That kind of connection can cut processing time by 25% or more.
The Hidden Cost of Compliance
For big companies, FDA compliance is a department. For small biotech startups, it’s a nightmare. The 2023 elimination of the de minimis exemption ($800 rule) hit research labs hard. Before, universities could ship small batches of experimental drugs or biological samples without paperwork. Now, every shipment-even a $200 vial of a new compound-requires full documentation. One academic center reported delays of 3-5 days per shipment, costing researchers weeks on critical experiments.
Small firms also struggle with cost. Hiring a customs broker to handle FDA paperwork runs $285-$450 per entry. For a startup shipping 10 times a month, that’s over $30,000 a year just in brokerage fees. And if one shipment gets detained because of a mislabeled box? The delay can cost hundreds of thousands in lost clinical trial timelines.
What Gets Caught-and What Doesn’t
The FDA’s system is good, but it’s not perfect. In 2022, a contaminated batch of valsartan (a blood pressure drug) slipped through because it came from a supplier not on the FDA’s radar. The drug was manufactured in China, labeled as compliant, and shipped under a low-risk classification. Lab tests later found a cancer-causing impurity. The FDA caught it after the product was already in U.S. pharmacies.
Another blind spot: counterfeit drugs sold online. The FDA estimates $4.3 billion worth of fake medications entered the U.S. in 2022. Most came from websites selling directly to consumers. These aren’t shipped through traditional ports-they’re mailed in small packages, often disguised as personal items. The FDA can’t monitor every eBay seller or Instagram pharmacy. That’s why the agency now works with the DEA and the FTC to shut down illegal online pharmacies.

What’s Changing in 2024 and Beyond
The FDA isn’t standing still. In 2024, it plans to expand the SSCPP to 50 companies, including contract manufacturers. It’s also testing blockchain tech to track drugs from factory to pharmacy. Pilot programs are underway to link manufacturing data with shipping records, making it harder to fake documentation.
Another big push: AI. The FDA is training machine learning models to predict which shipments are most likely to be violative. Early tests show a 25% improvement in targeting accuracy. That means fewer honest shipments get held up, and more bad ones get caught.
But resources are still tight. The Government Accountability Office found the FDA hasn’t fully implemented 13 of 17 key performance metrics required by law. And with over 1.2 million import entries each year, the agency can’t inspect everything. That’s why the system relies so heavily on trust-trust that manufacturers are honest, that paperwork is accurate, and that past behavior predicts future compliance.
What Importers Need to Get Right
If you’re shipping drugs into the U.S., here’s what you absolutely must do:
- Register your facility with the FDA (even if you’re overseas).
- List every product you export to the U.S. in the FDA’s Drug Listing System.
- Make sure labels meet 21 CFR Part 201 standards-English only, no missing warnings, no false claims.
- Use the FDA’s Electronic Entry Interface Repository (EEIR) to submit entries correctly. Errors here cause 28% of delays.
- Keep records for at least three years. The FDA can audit you anytime.
And don’t underestimate the power of communication. Call your local FDA port office before shipping. Ask who handles your product type. Ask if they’ve seen issues with your manufacturer before. A quick conversation can save you weeks.
Final Reality Check
The FDA’s import system is one of the most sophisticated in the world. It’s not flawless, but it’s far better than most other countries’. It saves lives by blocking tainted drugs, counterfeit insulin, and unapproved cancer treatments. But it’s also expensive, slow for small players, and still catching up to the rise of e-commerce drug sales.
For big companies, it’s a cost of doing business. For small labs and generic drug makers, it’s a hurdle that can make or break their supply chain. The system works best when everyone plays by the rules. When they don’t, the consequences aren’t just financial-they’re deadly.
Does the FDA inspect every drug shipment entering the U.S.?
No. The FDA physically inspects only about 1.2% of the over 100 million drug shipments entering the U.S. each year. Instead, it uses a risk-based system to screen nearly all entries electronically. High-risk shipments-those from manufacturers with past violations, from countries with weak oversight, or with incomplete paperwork-are flagged for physical inspection or lab testing.
What happens if a drug shipment gets detained by the FDA?
If a shipment is detained, it’s held at the port until the FDA makes a final decision. The importer has 10 days to fix the issue-like correcting a label or providing missing documentation. If the problem can’t be resolved, the FDA will refuse entry. The shipment may be destroyed, returned to the sender, or, in rare cases, reconditioned under FDA supervision. Repeated detentions can lead to an Import Alert, which automatically holds all future shipments from that manufacturer.
What is the Secure Supply Chain Pilot Program (SSCPP)?
The SSCPP is an FDA program that lets trusted manufacturers import up to five products with minimal inspection at U.S. ports. To qualify, a company must have a perfect compliance record for three straight years, pass a detailed audit, and demonstrate strong internal quality controls. Approved companies see clearance times drop from 7-10 days to under 48 hours. As of late 2023, only 27 manufacturers were in the program.
Why did the FDA eliminate the $800 de minimis exemption for drugs?
Before October 2023, low-value shipments under $800 were exempt from FDA review. This loophole was exploited to import dangerous substances like pill presses, fentanyl-laced capsules, and unapproved weight-loss drugs directly to consumers. The FDA eliminated the exemption to close this gap and bring all drug imports under the same safety standards-no matter the price or size of the shipment.
How can small biotech companies navigate the FDA import process?
Small companies should work with experienced customs brokers familiar with FDA requirements. They must ensure all documentation-commercial invoices, bills of lading, and Affirmations of Compliance-is perfect before submission. Using the FDA’s EEIR system and calling port-specific entry reviewers ahead of time can reduce delays. Many also apply for the SSCPP if they can meet the three-year compliance requirement. For research samples, planning shipments well in advance is critical, as delays can impact clinical trials.
Are generic drugs monitored as closely as brand-name drugs?
Not always. While brand-name drugs often come from well-known manufacturers with strong compliance histories, many generic drugs are sourced from overseas facilities with inconsistent records. In 2023, 37% of generic API shipments from certain Indian facilities were detained under Detention Without Physical Examination (DWPE), even when the manufacturer had no prior violations. The FDA is working to improve oversight, but industry surveys show pharmacy executives still consider generic drug supply chains less secure than brand-name ones.
What role does the DEA play in drug import inspections?
The DEA focuses on controlled substances-opioids, stimulants, sedatives, and other drugs with abuse potential. While the FDA checks for safety and labeling, the DEA ensures these drugs aren’t being smuggled in illegally. The two agencies share data, and shipments containing controlled substances are reviewed by both. A drug might pass FDA inspection but still be seized by the DEA if it lacks proper licensing or is being imported without authorization.








Diksha Srivastava
January 31, 2026 AT 00:15Sidhanth SY
January 31, 2026 AT 06:55Adarsh Uttral
February 2, 2026 AT 01:39Lisa McCluskey
February 3, 2026 AT 10:25April Allen
February 3, 2026 AT 20:44Amy Insalaco
February 4, 2026 AT 01:09Holly Robin
February 4, 2026 AT 09:51Blair Kelly
February 6, 2026 AT 07:48Natasha Plebani
February 8, 2026 AT 04:24calanha nevin
February 9, 2026 AT 13:47Lily Steele
February 10, 2026 AT 05:22Yanaton Whittaker
February 11, 2026 AT 15:02Russ Kelemen
February 12, 2026 AT 14:19Sarah Blevins
February 13, 2026 AT 18:55