Statins Interaction Checker
Check Your Statin Interactions
Results
Statins are among the most commonly prescribed drugs in the world. Millions of people take them every day to lower cholesterol and reduce the risk of heart attacks and strokes. But not all statins work the same way when mixed with other medications. Some can cause dangerous side effects - like muscle damage or even rhabdomyolysis - when taken with common drugs like antibiotics, blood pressure pills, or even supplements. The key to staying safe isn’t just taking your statin. It’s knowing which statin you’re on and how it behaves with everything else in your medicine cabinet.
Why Some Statins Are Riskier Than Others
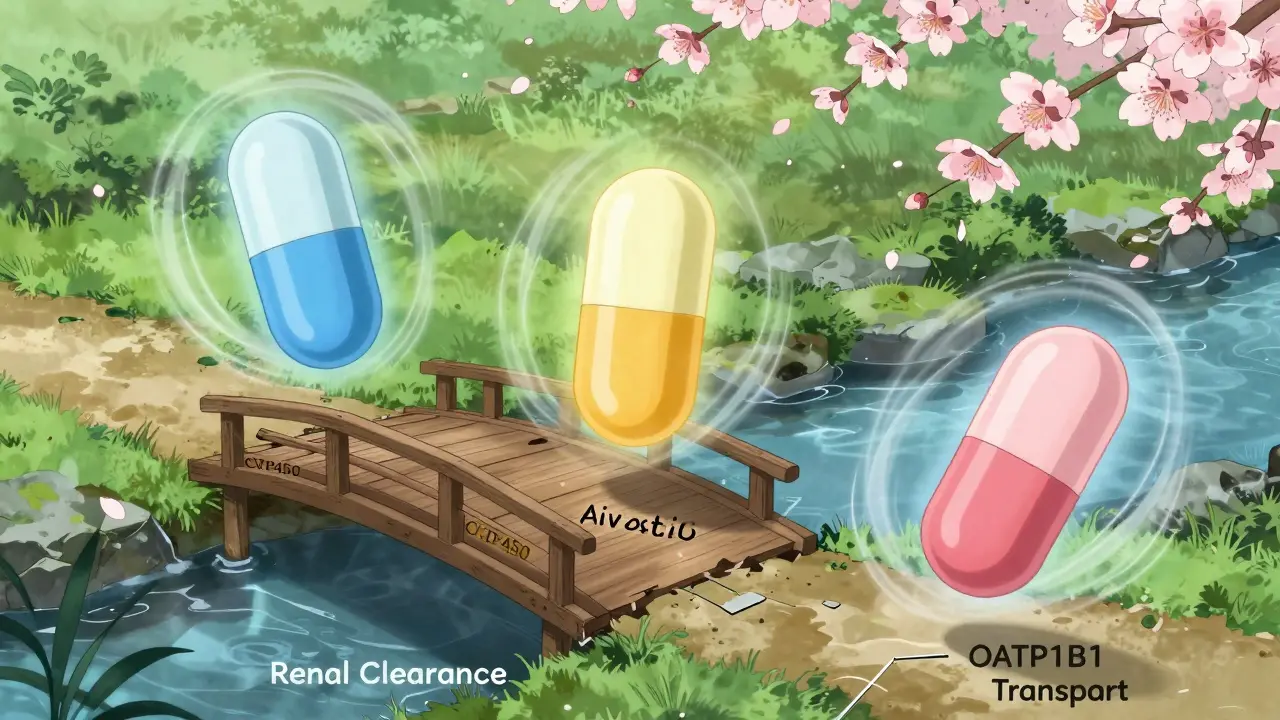
There are seven statins approved for use in the U.S.: atorvastatin, simvastatin, pravastatin, lovastatin, fluvastatin, rosuvastatin, and pitavastatin. They all do the same basic job - block an enzyme called HMG-CoA reductase to lower LDL (bad) cholesterol. But how your body processes each one changes everything. The biggest factor? How they’re broken down. Five of them - simvastatin, lovastatin, atorvastatin, fluvastatin, and the withdrawn cerivastatin - rely heavily on liver enzymes called CYP450. That’s where problems start. If another drug blocks those enzymes, the statin builds up in your blood. Think of it like a clogged drain. The statin doesn’t get washed away, so it piles up. That’s when muscle pain, weakness, or worse can happen. Simvastatin and lovastatin are the most vulnerable. When taken with clarithromycin (an antibiotic), simvastatin levels can spike by 10 times. Lovastatin? Up to 16 times higher. That’s not a typo. That’s a medical emergency waiting to happen. Both are also banned with cyclosporine (used after organ transplants) because the risk of muscle breakdown is too high. Atorvastatin is less risky but still needs caution. With clarithromycin, its levels can jump 4 times. With diltiazem or verapamil (blood pressure meds), the increase is 3 to 8 times. That’s why doctors often limit atorvastatin to 10 mg or less if you’re on those drugs. Then there are the statins that barely touch CYP enzymes: pravastatin, rosuvastatin, and pitavastatin. These are much safer. Pravastatin is mostly cleared by the kidneys. Rosuvastatin uses a mix of pathways, including a transporter called OATP1B1. Pitavastatin is mostly handled by glucuronidation. None rely heavily on CYP3A4 - the most commonly blocked enzyme. That’s why they’re often the go-to choice for people on multiple medications.The Hidden Culprit: Transporter Proteins
It’s not just about liver enzymes. There’s another player: OATP1B1. This protein shuttles statins into liver cells so they can do their job. If something blocks it, the statin stays in your bloodstream longer - and that’s trouble. Cyclosporine is the worst offender. It blocks OATP1B1 so hard that it can increase rosuvastatin levels by 7.1 times and pitavastatin by the same amount. That’s why cyclosporine is absolutely off-limits with pitavastatin and lovastatin. Even pravastatin, which is usually safe, needs a max dose of 40 mg when taken with cyclosporine. Other drugs that block OATP1B1 include some HIV meds, certain antifungals, and even high-dose niacin. If you’re on any of these, your doctor needs to know which statin you’re taking - and whether it’s the right one.Statins and Common Medications: What to Watch For
Let’s look at real-world combinations you might actually encounter:- Antibiotics: Clarithromycin and erythromycin are big red flags for simvastatin and lovastatin. Azithromycin is safer. Always ask your pharmacist if your antibiotic interacts with your statin.
- HIV Medications: Drugs like atazanavir, darunavir, and ritonavir are CYP3A4 inhibitors. They’re dangerous with simvastatin and lovastatin. Pravastatin and rosuvastatin are better choices - but even then, dose reductions may be needed.
- Blood Pressure Pills: Diltiazem and verapamil (calcium channel blockers) can double or triple statin levels. Avoid simvastatin and lovastatin entirely. Atorvastatin can be used at low doses with monitoring.
- Fibrates: Gemfibrozil is the worst. It blocks the enzymes and transporters that clear statins. Never pair it with simvastatin, lovastatin, or atorvastatin. Fenofibrate is much safer and is often recommended instead.
- Colchicine: Used for gout, colchicine can increase muscle toxicity risk when combined with statins. The risk is low with pravastatin or rosuvastatin, but your doctor may still lower your statin dose or check your muscle enzymes.
- Ticagrelor: This blood thinner (used after heart attacks) slightly increases atorvastatin levels. It’s usually okay. But with simvastatin or lovastatin, the dose must stay under 40 mg/day.

Who’s Most at Risk?
Not everyone who takes a statin with a risky drug will have problems. But some people are more vulnerable:- Older adults (over 65)
- People with kidney or liver disease
- Those taking multiple medications
- People with low body weight
- Those with a genetic variation in the SLCO1B1 gene - which affects how well OATP1B1 works
What Should You Do?
If you’re on a statin and start a new medication - even an over-the-counter one - talk to your doctor or pharmacist. Don’t assume it’s safe. Here’s what to ask:- Is this new drug known to interact with statins?
- Which statin is safest for me right now?
- Do I need a lower dose?
- Should I get my muscle enzymes checked?
Monitoring and Safety
Your doctor should check your liver enzymes and creatine kinase (CK) before you start a statin, especially if you’re on other meds. Muscle pain, weakness, or dark urine? Call your doctor immediately. These could be signs of rhabdomyolysis - a rare but life-threatening condition. Regular check-ins matter. A 2022 American College of Cardiology guideline says: don’t just set it and forget it. If you start a new drug, re-evaluate your statin. If you’re on multiple meds, consider a statin with the lowest interaction risk - pravastatin or rosuvastatin.What’s Changing?
Newer drugs like bempedoic acid (Nexletol) are being used as statin alternatives. They lower LDL without the same interaction risks. In the CLEAR Outcomes trial, bempedoic acid cut major heart events by 17% in people who couldn’t tolerate statins. It’s not a replacement for everyone - but for those with complex drug regimens, it’s a real option. Research is also moving toward personalized medicine. The NIH is funding tools that use your genes, age, weight, and current meds to predict which statin is safest for you. In the next 5 years, we may see pharmacogenetic testing become part of routine care for statin users.Bottom Line
Statins save lives. But their safety depends on the right match. Simvastatin and lovastatin are powerful - but risky with common drugs. Pravastatin and rosuvastatin are quieter, safer choices for people on multiple medications. Atorvastatin is in the middle - fine if used carefully. Don’t assume all statins are equal. Ask your doctor: Is this the safest statin for me - right now?Can I take grapefruit juice with my statin?
Grapefruit juice blocks the CYP3A4 enzyme, which can raise statin levels. It’s safest with pravastatin or rosuvastatin. With simvastatin or lovastatin, even one glass can double your statin levels. Atorvastatin is also affected - but less so. If you like grapefruit, ask your doctor if switching statins is a better option than giving up your morning juice.
Why is simvastatin 80 mg no longer recommended?
The 80 mg dose of simvastatin was linked to a higher risk of muscle damage, especially in the first 12 months. Studies showed no extra heart benefit compared to lower doses, but the risk of rhabdomyolysis went up. The FDA and American Heart Association now recommend avoiding it entirely. If you’re on 80 mg, talk to your doctor about switching.
Can I take a statin if I have kidney disease?
Yes - but not all statins are equal. Pravastatin and rosuvastatin are cleared by the kidneys, so dose adjustments are needed. Simvastatin and lovastatin are safer in kidney disease because they’re processed by the liver. But if you’re also on other drugs that interact with statins, even pravastatin may need a lower dose. Your doctor will check your kidney function and adjust accordingly.
Do I need to stop my statin before surgery?
Generally, no. Stopping your statin before surgery increases your risk of heart problems. Most guidelines now say to keep taking it, even before major procedures. The exception is if you’re on a high-risk combo (like simvastatin with an antibiotic) or if you’re having heart surgery. Always check with your surgeon and cardiologist - don’t stop on your own.
Is there a statin that doesn’t interact with anything?
No statin is completely free of interactions. But pravastatin comes closest. It’s not metabolized by CYP enzymes, and it’s not strongly affected by OATP1B1 blockers. It’s often the top choice for people on multiple medications, including HIV drugs, transplant meds, or blood thinners. Rosuvastatin is a close second - but watch out for cyclosporine. If you’re on a complex drug list, pravastatin is usually the safest bet.