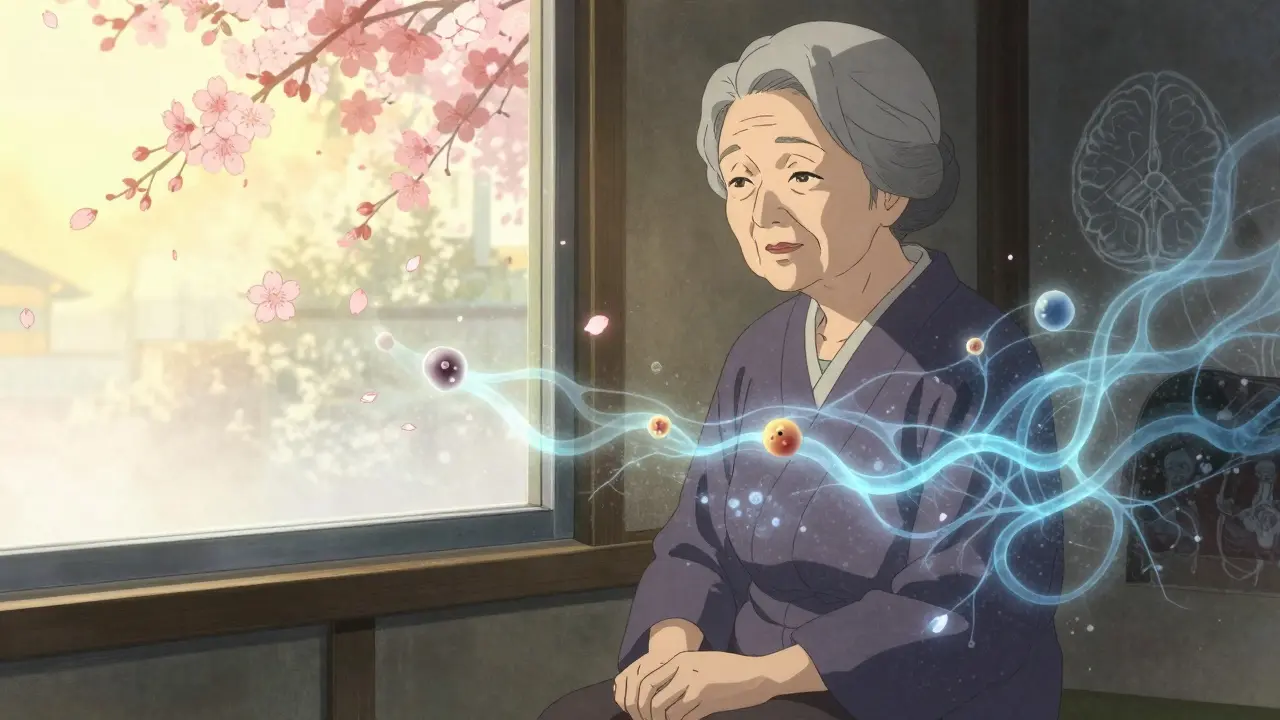
Alzheimer’s disease isn’t just forgetting where you put your keys. It’s losing the ability to recognize your own children, forgetting how to tie your shoes, or no longer remembering the name of the person you’ve been married to for 50 years. It’s the most common cause of dementia, affecting 7.2 million Americans over 65 - and that number is expected to nearly double by 2060. This isn’t normal aging. It’s a brutal, progressive brain disease that slowly erases who you are.
What Happens in the Brain?
At its core, Alzheimer’s is defined by two visible abnormalities in the brain: amyloid plaques and neurofibrillary tangles. Amyloid plaques are sticky clumps of a protein called beta-amyloid that build up between nerve cells. Neurofibrillary tangles are twisted fibers of a protein called tau that accumulate inside cells. These aren’t just bystanders - they actively kill brain cells, especially in areas responsible for memory and thinking, like the hippocampus and cerebral cortex.
By the time someone shows clear symptoms, significant damage has already occurred. Brain scans now show that these changes can start decades before memory problems become obvious. That’s why researchers are pushing hard for earlier detection. Biomarkers - measurable signs of the disease - are now part of the diagnostic process. Cerebrospinal fluid tests can detect low levels of amyloid-beta 42 and high levels of phosphorylated tau. Amyloid PET scans, which light up plaques in the brain, are 92% specific. But here’s the catch: only 35% of U.S. healthcare facilities offer these scans. Many patients wait months, or even years, for a definitive diagnosis.
The Seven Stages of Progression
Alzheimer’s doesn’t hit all at once. It creeps in, then escalates. Experts break it down into seven stages:
- Stage 1: No impairment. No noticeable symptoms. Brain changes may already be happening.
- Stage 2: Very mild decline. Minor memory lapses - forgetting names, misplacing things. Often dismissed as stress or aging.
- Stage 3: Mild decline. Friends and family start noticing. Trouble remembering recent conversations, planning events, or finding the right words.
- Stage 4: Moderate decline. Clear signs of dementia. Forgetting personal history, difficulty managing money, becoming withdrawn. This is often when people get diagnosed.
- Stage 5: Moderately severe decline. Needs help with daily tasks. May forget where they are, what year it is, or the names of close relatives. Can still recall basic personal info.
- Stage 6: Severe decline. Major personality changes. May not recognize loved ones. Needs help with dressing, bathing, using the toilet. Incontinence becomes common. Sleep disturbances and agitation increase.
- Stage 7: Very severe decline. Loses ability to speak, walk, or swallow. Completely dependent. The body begins to shut down.
On average, people live 4 to 8 years after diagnosis, but some survive up to 20 years. The pace varies wildly - and no one can predict exactly how fast it will move for any individual.
Current Medications: What Works - and What Doesn’t
For decades, the only treatments available were drugs that offered temporary, modest relief. Cholinesterase inhibitors - donepezil, rivastigmine, and galantamine - work by boosting acetylcholine, a brain chemical involved in memory. They help about 40-50% of patients stabilize symptoms for 3 to 6 months. But they don’t stop the disease. Side effects like nausea, vomiting, and diarrhea are common. One caregiver in Florida described how her mother’s sleep worsened and she became nauseous on donepezil - the downsides outweighed any benefit.
Memantine, an NMDA receptor antagonist, is used in moderate to severe cases. It helps regulate glutamate, a brain chemical that can damage neurons when overactive. It slows decline by 20-30% in some patients, but again, it’s not a cure.
These drugs are like putting a bandage on a broken leg. They help with symptoms, but the underlying damage keeps spreading.

The New Wave: Disease-Modifying Therapies
In January 2025, everything changed. The FDA gave full approval to lecanemab (brand name Leqembi), the first drug proven to slow the progression of Alzheimer’s, not just mask symptoms. In the CLARITY AD trial with nearly 1,800 patients, lecanemab reduced cognitive decline by 27% over 18 months. Another drug, donanemab, showed an even stronger 35% slowing of decline in its Phase 3 trial.
These are monoclonal antibodies. They work by targeting and clearing amyloid plaques from the brain. For the first time, we have drugs that actually alter the disease’s course - if caught early enough.
But they come with serious risks. About 12.5% of people on lecanemab and 24% on donanemab develop ARIA - amyloid-related imaging abnormalities. This means brain swelling or tiny bleeds. It’s often asymptomatic, but can be dangerous. That’s why patients need monthly MRI scans for the first year. Many families are overwhelmed by the logistics. On Reddit, 72% of posts about lecanemab mention the stress of frequent MRIs.
There’s also the cost. Lecanemab runs about $26,500 per year. Medicare covers it, but only under strict conditions. Only 3% of eligible patients in the U.S. have received it so far - not because it doesn’t work, but because the system isn’t ready. Specialized centers, trained staff, and imaging infrastructure are scarce. Just 15% of eligible patients are getting these treatments.
What About Oral Options?
There’s hope on the horizon. ALZ-801, an oral prodrug of tramiprosate, showed an 81% reduction in cognitive decline in patients with two copies of the APOE4 gene - the strongest genetic risk factor for late-onset Alzheimer’s. This is huge. It means future treatments could be tailored to genetic profiles. Imagine a simple blood test telling you which drug is right for you.
Other drugs are targeting tau protein, inflammation, and metabolic dysfunction. As of early 2025, 127 clinical trials are testing non-amyloid approaches. The field is moving beyond the amyloid hypothesis. Combination therapies - hitting multiple targets at once - are the next frontier.
Non-Drug Approaches That Actually Help
Medications aren’t the whole story. Lifestyle changes have real, measurable power. The FINGER study - a landmark trial in Finland - showed that combining diet, exercise, cognitive training, and managing blood pressure and cholesterol reduced cognitive decline by 25% over two years. People didn’t need drugs. They needed structure, support, and consistency.
Cognitive stimulation therapy (CST), where people engage in group activities like memory games, music, and discussions, improved cognitive scores by 1.5 points on the ADAS-cog scale in a 2024 meta-analysis. That’s not a cure - but it’s meaningful. It helps people stay connected, engaged, and less isolated.
And then there’s prevention. Dr. Carol Brayne from Cambridge University says up to 40% of dementia cases could be prevented or delayed by managing nine modifiable risks: high blood pressure, obesity, hearing loss, smoking, depression, physical inactivity, diabetes, low education, and social isolation. Many of these are controllable in midlife. What you do at 50 matters for your brain at 75.
The Human Cost: Caregivers on the Front Lines
Behind every patient is a caregiver - often a spouse, child, or sibling - who’s drowning. Eighty-five percent report high emotional stress. Forty percent show signs of depression. Sixty percent cut back on work. The average annual income loss for caregivers is $18,200.
Access to care is uneven. Sixty-eight percent of caregivers surveyed in 2025 said insurance denied their request for amyloid PET scans. Out-of-pocket costs for diagnostics and treatments often exceed $1,000. Rural families have it worse - 78% of certified treatment centers are in urban areas.
And there’s a glaring gap in diversity. Only 8% of participants in recent amyloid therapy trials are non-white, even though dementia affects Black and Hispanic populations at higher rates. Without diverse trials, we don’t know if these drugs work equally well for everyone.
What’s Next?
The future isn’t one drug. It’s precision medicine. Blood tests that detect Alzheimer’s years before symptoms - like the PrecivityAD2 test, which matches amyloid PET scans with 97% accuracy - could make screening as simple as a blood draw. Instead of $5,000 for a PET scan, it could cost $500.
By 2030, we may match patients to treatments based on their genetic makeup, biomarker profile, and overall health. Someone with APOE4 might get ALZ-801. Someone with high inflammation might get an anti-inflammatory combo. Someone with vascular risk factors might get a lifestyle plan paired with a low-dose drug.
The Alzheimer’s Association says we’re not at the finish line - but we’re finally on the track. We have tools to detect it earlier. We have drugs that slow it. We have proven ways to support people and their families. The challenge now isn’t just science - it’s access, equity, and building a system that can deliver these advances to everyone who needs them.
One thing is certain: Alzheimer’s isn’t going away. But we’re no longer powerless against it.
Can Alzheimer’s be cured?
No, Alzheimer’s cannot be cured yet. But new disease-modifying drugs like lecanemab and donanemab can slow cognitive decline by 25-35% in early-stage patients. These are the first treatments proven to change the disease’s course, not just manage symptoms. Research is moving fast, and combination therapies targeting multiple brain pathways are in development.
How do you know if someone has Alzheimer’s and not just normal aging?
Normal aging means occasionally forgetting a name or where you parked. Alzheimer’s means forgetting the name of your spouse, getting lost in your own neighborhood, or repeating the same question multiple times in a single conversation. If memory loss disrupts daily life - managing bills, cooking, taking medication - it’s not normal. A doctor can use cognitive tests, brain scans, and biomarkers to distinguish between normal aging and Alzheimer’s.
Are the new Alzheimer’s drugs worth the risk and cost?
It depends. For someone in the early stage with confirmed amyloid plaques, the 27-35% slowing of decline can mean months or years of preserved independence. But the drugs carry a 12-24% risk of brain swelling or bleeding, require monthly MRIs, and cost $26,500 a year. For many families, the emotional and logistical burden outweighs the benefit. Doctors now recommend these drugs only for early-stage patients with confirmed biomarkers - not for late-stage or unconfirmed cases.
Can lifestyle changes really prevent Alzheimer’s?
Yes - and not just delay it. The FINGER study showed a 25% reduction in cognitive decline over two years with a combination of healthy diet, regular exercise, cognitive training, and managing blood pressure and cholesterol. Other studies link hearing loss, social isolation, and untreated depression to higher dementia risk. Managing these factors in midlife can reduce your risk by up to 40%. It’s not a guarantee, but it’s the best defense we have right now.
Why are so few people getting the new Alzheimer’s drugs?
Because the system isn’t ready. These drugs require certified treatment centers, specialized MRI scans, trained staff, and ongoing monitoring. Only 35% of U.S. facilities offer amyloid PET scans. Most are in big cities. Insurance approvals are slow. The learning curve for doctors is 6-9 months. Only 15% of eligible patients are receiving them. It’s not that the drugs don’t work - it’s that access is broken.
Is Alzheimer’s genetic?
Most cases - about 90% - are late-onset with no clear inheritance pattern. But having one copy of the APOE-e4 gene increases risk 3-4 times. Two copies raise it up to 15 times. There are also rare early-onset forms caused by specific gene mutations (like in APP, PSEN1, PSEN2), which are inherited. Genetic testing is available, but it’s not recommended for everyone. Knowing your APOE status can help guide prevention and future treatment choices.






LOUIS YOUANES
January 29, 2026 AT 12:20Megan Brooks
January 31, 2026 AT 01:59Paul Adler
February 1, 2026 AT 14:39Kristie Horst
February 2, 2026 AT 20:16Andy Steenberge
February 3, 2026 AT 08:56Laia Freeman
February 3, 2026 AT 10:21rajaneesh s rajan
February 5, 2026 AT 04:30paul walker
February 5, 2026 AT 13:32