Herbal Supplement Interaction Checker
Check for Dangerous Interactions
Select your prescription medications and we'll check for potential dangerous interactions with common herbal supplements.
Every year, thousands of Americans take herbal supplements thinking they’re harmless - just natural, plant-based remedies. But what many don’t realize is that some of these products contain hidden drugs, contaminants, or ingredients that can clash dangerously with prescription medications. The FDA doesn’t approve herbal supplements before they hit store shelves. That means you’re on your own when it comes to safety - unless you talk to your doctor.
What the FDA Actually Does (and Doesn’t Do)
The FDA treats herbal supplements like food, not medicine. That means companies don’t need to prove they work or are safe before selling them. All they have to do is slap on a label that says: "This statement has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease." It’s a legal loophole that lets products with no clinical backing stay on shelves for years.
Between 2007 and 2016, researchers found 776 dietary supplements containing undeclared pharmaceutical drugs. Some had weight-loss pills disguised as herbal fat burners. Others had erectile dysfunction drugs hidden in "natural" male enhancement formulas. One study in JAMA Internal Medicine found that 15% of tested supplements contained active drugs not listed on the label. These aren’t rare cases - they’re routine.
And it’s not just about hidden drugs. A 2021 case report in the Journal of Clinical Pharmacy and Therapeutics described a patient on blood thinners who started taking ginkgo biloba. No one told their doctor. The result? Severe internal bleeding. Ginkgo thins the blood. So does warfarin. Together? A dangerous combo.
Herbal Products That Can Be Dangerous Without Disclosure
Not all herbal supplements are risky. But some are known troublemakers. Here are the top ones the FDA and medical experts warn you to disclose to your doctor:
- St. John’s Wort - Often used for mild depression, this herb can make birth control pills, antidepressants, blood thinners, and even HIV meds stop working. It speeds up how fast your liver breaks down drugs, so they never reach their target.
- Ginkgo Biloba - Marketed for memory and circulation, it can increase bleeding risk when taken with aspirin, ibuprofen, or warfarin. It’s been linked to surgical complications and brain hemorrhages.
- Garlic Supplements - While garlic in food is fine, concentrated supplements can thin your blood. If you’re scheduled for surgery or on anticoagulants, even a few extra pills can turn a routine procedure into a life-threatening event.
- Kava - Used for anxiety, kava has been tied to severe liver damage. The FDA issued a consumer advisory in 2002, and it’s still on the list of high-risk products.
- Green Tea Extract - Sold for weight loss and antioxidants, it’s caused acute liver failure in at least 20 documented cases. Most victims were taking high-dose capsules, not drinking tea.
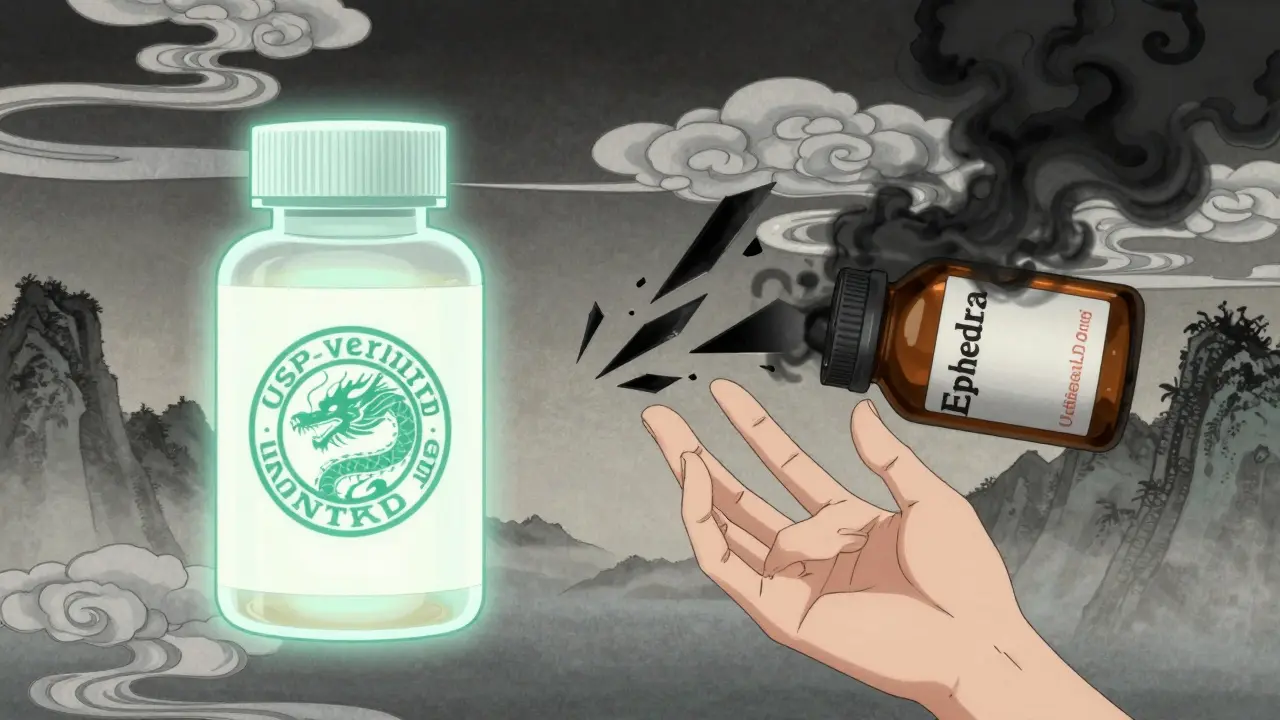
- Ephedra (Banned, But Still Out There) - The FDA banned ephedra in 2004, but counterfeit versions still pop up in weight-loss and bodybuilding products. It raises blood pressure, triggers heart attacks, and can cause strokes.
These aren’t "maybe" risks. They’re documented dangers. And they’re not always obvious on the label.

Why Doctors Need to Know What You’re Taking
Here’s the hard truth: most doctors don’t ask about supplements. And most patients don’t volunteer the info. A 2022 survey of 1.5 million physicians found that 68% encounter patients who hide supplement use. Why? Because patients think supplements are "safe" or "not medicine." They don’t realize their herbal tea could interfere with their heart medication.
At Johns Hopkins Hospital, doctors tried a simple fix: they started asking five clear questions during every intake:
- Are you taking any vitamins or supplements?
- What are you taking them for?
- How much are you taking?
- How often?
- Have you noticed any side effects?
Before this, only 32% of patients disclosed supplement use. After six months? It jumped to 78%. Simple questions save lives.
Supplement interactions aren’t just theoretical. They’re happening in ERs right now. A 2021 FDA report showed that over 14,000 adverse events from supplements were reported between 2018 and 2022. The top complaints? Stomach problems, heart palpitations, dizziness, and liver damage. Many of those cases involved herbs taken with prescription drugs.
How to Spot a Dangerous Product
Not all herbal products are created equal. Here’s how to tell the safe ones from the risky ones:
- Check for third-party verification - Look for the USP Verified Mark, NSF Certified, or ConsumerLab.com seal. These groups test products independently. USP-verified supplements meet strict standards for purity and potency. Non-verified products fail label claims 33% of the time.
- Read the label - Ingredients should be listed in order of amount. Botanicals should have their Latin names (e.g., Hypericum perforatum for St. John’s Wort). If it just says "herbal blend," walk away.
- Watch out for claims - If a product says it "treats diabetes," "cures cancer," or "boosts immunity," it’s breaking FDA rules. Real supplements can’t make those claims.
- Search the FDA’s warning list - The FDA updates its warning letter database weekly. Type in the brand name. If it’s been flagged, don’t buy it.
Amazon reviews aren’t reliable. A 2021 study of 500,000 supplement reviews found that 18% mentioned side effects - but most people don’t report them. Just because a product has 4.5 stars doesn’t mean it’s safe.
What You Should Do Right Now
You don’t need to stop taking supplements. But you do need to be smart about them.
- Talk to your doctor - Before starting any new herb, ask: "Could this interact with my medications?" Bring the bottle. Don’t rely on memory.
- Use the FDA’s Safety Reporting Portal - If you have a bad reaction, report it. Even if it’s "just" nausea or a rash. The FDA needs this data to track dangerous products.
- Download the NCCIH app - The National Center for Complementary and Integrative Health offers a free app with 1,200+ evidence-based fact sheets on herbs, vitamins, and supplements. No ads. No marketing. Just science.
- Choose verified brands - Look for USP, NSF, or ConsumerLab. They cost a little more, but they’re far less likely to contain hidden drugs or contaminants.
The supplement industry is worth over $50 billion. That’s a lot of money, and not all of it’s going toward safety. Your health shouldn’t be a gamble. If you’re taking herbs - especially if you’re on prescription meds - disclosure isn’t optional. It’s essential.
Do herbal supplements need FDA approval before being sold?
No. Unlike prescription drugs, herbal supplements don’t need FDA approval before they go on the market. Manufacturers only need to notify the FDA if they’re using a new dietary ingredient. They don’t have to prove the product is safe or effective. The FDA only steps in after a product is found to be harmful, mislabeled, or contaminated.
Can herbal supplements interact with prescription medications?
Yes - and these interactions can be life-threatening. St. John’s Wort can make birth control, antidepressants, and blood thinners less effective. Ginkgo biloba and garlic supplements can increase bleeding risk when taken with aspirin or warfarin. Green tea extract has caused liver failure in people taking high doses. Always tell your doctor what herbs you’re using.
Are "natural" herbal products always safe?
No. "Natural" doesn’t mean safe. Kava has caused liver failure. Green tea extract has led to acute liver damage. Ephedra - a banned herb - still shows up in illegal weight-loss products. Many herbal supplements contain hidden drugs, heavy metals, or pesticides. Just because something comes from a plant doesn’t mean it’s harmless.
How can I tell if my supplement is safe?
Look for third-party verification seals like USP, NSF, or ConsumerLab.com. These organizations test products for purity, potency, and contamination. Check the FDA’s warning letter database for your brand’s name. Avoid products with vague claims like "cures cancer" or "boosts immunity." Always read the full ingredient list - especially Latin names for herbs.
Should I stop taking herbal supplements if I’m on medication?
Not necessarily - but you must talk to your doctor first. Some herbs are safe to take with certain medications. Others aren’t. Never assume an herb is harmless just because it’s sold in a store. Your pharmacist or doctor can check for interactions. When in doubt, pause use until you get professional advice.




Sarah Barrett
February 15, 2026 AT 05:50It’s wild how we treat supplements like they’re harmless tea, when half of them could be chemical cocktails in disguise. I had a friend take a "natural" energy booster and ended up in the ER with a racing heart-turns out, it had unlisted caffeine analogs. The label just said "herbal blend." No Latin names. No dosage. Just vibes and promises.
And yet, we scroll through Amazon reviews like they’re peer-reviewed journals. Four stars because it "changed my life"? Meanwhile, three people mentioned liver pain in the fine print. We’re not just naive-we’re actively ignoring the red flags.
The FDA’s hands are tied because of how the law’s written. It’s not about oversight; it’s about profit margins. Companies know the loophole. They exploit it. And we’re the ones paying with our health.
I started asking my pharmacist to scan every bottle before I buy. She laughs, then hands me the USP seal guide. It’s the only thing that gives me peace now.
Knowledge isn’t power here. Verification is.
Josiah Demara
February 15, 2026 AT 09:07This article is a masterclass in fearmongering dressed up as public service. Let me guess-you’re one of those people who thinks every supplement is a ticking time bomb because a few bad actors exist. That’s not caution-that’s paranoia with a thesaurus.
St. John’s Wort? Yes, it interacts. So does grapefruit. Should we ban grapefruit? No-we educate. But no one wants to educate anymore. They want to scare you into buying only FDA-approved drugs-which are 10x more expensive and just as likely to cause side effects.
Green tea extract caused liver damage? In 20 cases out of billions of doses. That’s statistically negligible. Meanwhile, pharmaceuticals kill 250,000 Americans a year. Where’s the outcry for that?
You’re not protecting people. You’re feeding a pharmaceutical monopoly. And you’re making millions believe they need permission from a doctor to take a vitamin. Pathetic.
Kaye Alcaraz
February 15, 2026 AT 16:27Thank you for this clear, vital guide. I’ve been a nurse for 18 years and I can tell you-every single time a patient says "I just take this herb, it’s natural," it’s the one thing we didn’t know that nearly killed them.
One woman on warfarin took ginkgo because she read it "improves memory." She had a subdural hemorrhage during a fall. She survived. But her brain will never be the same.
Doctors don’t ask because they’re rushed. Patients don’t tell because they’re embarrassed. We need to normalize this conversation like we do with smoking or alcohol.
Bring your bottle. Write it down. Say it out loud. Your doctor isn’t judging you-they’re trying to keep you alive.
And yes-USP, NSF, ConsumerLab. Pay the extra five bucks. It’s cheaper than an ER visit.
Thank you for saying what needs to be said.
Charlotte Dacre
February 15, 2026 AT 19:49Oh wow. So now we’re treating herbal supplements like they’re nuclear codes? "Don’t take garlic unless you’ve filled out a 12-page form and gotten approval from your internist?"
Meanwhile, in the real world, people have been chewing willow bark for 5,000 years. That’s aspirin, by the way. Nature didn’t wait for FDA approval to heal humans.
It’s not about safety. It’s about control. The pharmaceutical industry doesn’t want you to have alternatives. So they paint everything natural as a death trap. Convenient, isn’t it?
Next they’ll ban sunlight because UV rays "can interact with your meds."
Chiruvella Pardha Krishna
February 15, 2026 AT 23:00There is a metaphysical truth here, beyond the pharmacological data. The body does not exist in isolation-it is a vessel of energy, of subtle currents, of ancestral wisdom. To reduce herbalism to chemical interactions is to reduce the soul to a neurotransmitter.
Yet, we live in an age of mechanistic medicine, where every root, every leaf, must be dissected, quantified, and approved by bureaucrats who have never touched soil.
Is it not tragic that we fear the healing power of the earth, yet willingly swallow synthetic molecules with unknown long-term effects?
The real danger is not the herb-but the loss of trust in nature’s intelligence.
Perhaps the FDA’s greatest failure is not its oversight-but its arrogance.
Virginia Kimball
February 16, 2026 AT 07:09YES. I used to think supplements were just fancy vitamins until my mom had a bad reaction to kava. She didn’t tell her doctor because she didn’t think it counted. Now she only uses USP-certified stuff and brings every bottle to appointments. It’s awkward at first, but it saved her life.
Also-NCCIH app is a game changer. Free. No ads. Just facts. I wish I’d known about it years ago.
Don’t be scared. Be smart. Talk. Bring the bottle. You’ve got this.
Kapil Verma
February 16, 2026 AT 17:11Western medicine is a scam. You think the FDA protects you? They protect Big Pharma. In India, we’ve used turmeric, ashwagandha, and tulsi for centuries without a single regulation. No one dies. No one goes to the ER. Why? Because we trust nature, not corporate labs.
You Americans are so scared of your own shadows. A little herb? A little garlic? You need a 10-step checklist? Pathetic. Your bodies are weak because your minds are weak.
Stop listening to fear-mongers. Go back to the roots. Real healing doesn’t come from a bottle with a USP seal. It comes from tradition.
Michael Page
February 18, 2026 AT 06:20I’ve been reading about this for months. The data is overwhelming. What’s more disturbing is how little we talk about it. We’re told to be mindful of our diet, our sleep, our mental health-but not what’s in that capsule on the shelf next to the protein powder.
There’s a silence here. A cultural silence. We don’t ask. We don’t investigate. We assume.
It’s not ignorance. It’s avoidance.
And avoidance kills.
Betty Kirby
February 19, 2026 AT 22:39Let’s be real-the supplement industry is a gold rush. 776 products with hidden drugs? That’s not negligence. That’s criminal. And yet, the FDA only acts after people die. That’s not oversight. That’s a waiting game.
And don’t get me started on Amazon reviews. I bought a "natural" weight loss pill based on 4.8 stars. Turned out it had sibutramine-banned in 2010. I had a panic attack. My doctor said I was lucky I didn’t have a stroke.
There’s no ethics here. Just profit. And we’re the collateral.
Erica Banatao Darilag
February 21, 2026 AT 11:29