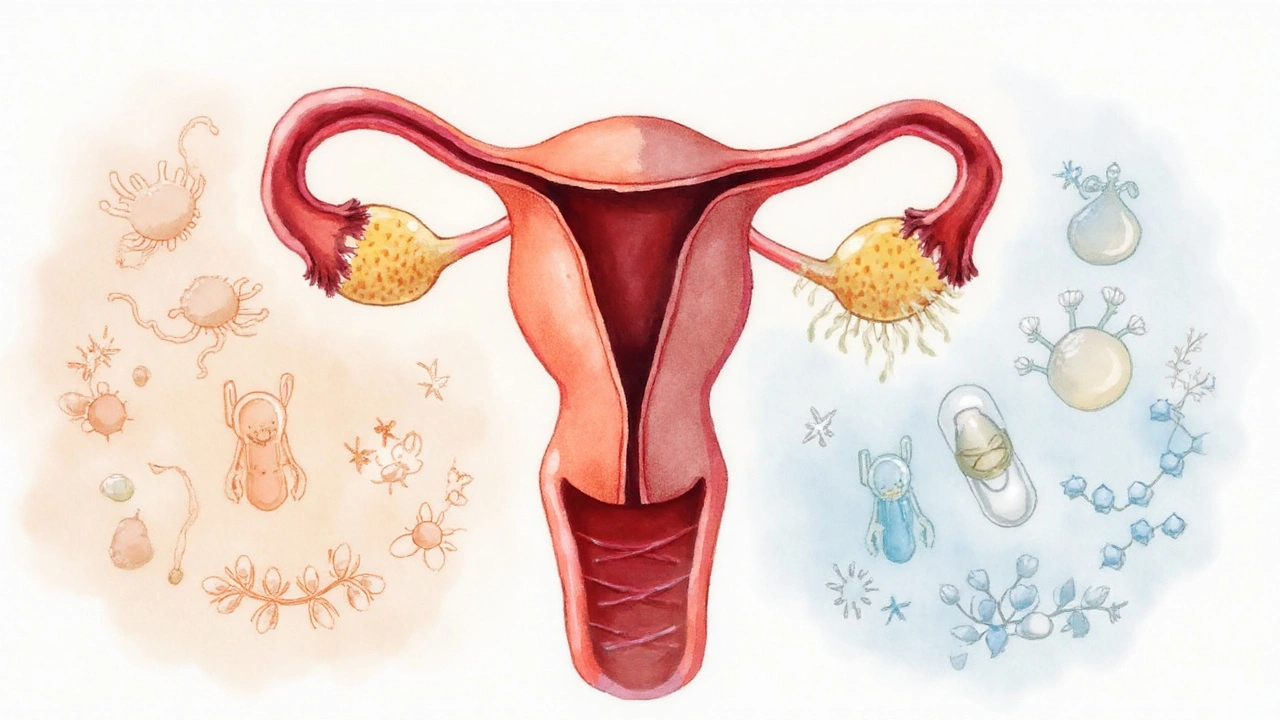
Intrauterine Device (IUD) is a small, T‑shaped contraceptive placed inside the uterus that provides long‑term birth control (3‑10years) without daily pills.
Vaginal infection refers to any disruption of the normal vaginal microbiome that causes symptoms such as discharge, itching, or odor. Common forms include bacterial vaginosis and candidiasis.
Copper IUD is a non‑hormonal device that releases copper ions to create a spermicidal environment. It typically lasts up to 10years.
Hormonal IUD releases levonorgestrel, a progestin that thickens cervical mucus and thins the uterine lining. Effective for 3‑7years depending on the brand.
Bacterial vaginosis (BV) is a condition where anaerobic bacteria overgrow, reducing protective Lactobacillus species. It is the most common vaginal infection in reproductive‑age women.
Candidiasis (yeast infection) is a fungal overgrowth of Candida species, often triggered by antibiotic use or hormonal shifts.
Pelvic inflammatory disease (PID) is a infection of the upper reproductive tract that can follow untreated vaginal infections. Early detection is crucial.
Biofilm formation describes the ability of bacteria to adhere to the IUD surface and create a protective matrix, making infections harder to treat.
Quick Takeaways
- Both copper and hormonal IUDs can alter vaginal flora, but the overall infection risk remains low.
- Hormonal IUDs slightly increase yeast infection rates; copper IUDs are more linked to bacterial vaginosis.
- Proper insertion technique and routine check‑ups cut the chance of biofilm‑related complications.
- Early symptoms-unusual discharge, itching, or odor-should prompt a clinician visit.
- Good hygiene, probiotic use, and avoiding douching help keep the vaginal ecosystem balanced.
How IUDs Interact with the Vaginal Microbiome
The uterus and vagina share a delicate microbial balance. When an IUD is placed, its material becomes a foreign surface inside the uterus. Over time, bacteria can adhere, forming a biofilm. This process is more common with copper because the metal ions can attract anaerobic organisms, while levonorgestrel in hormonal IUDs subtly changes cervical mucus, sometimes favoring yeast growth.
Studies from 2022‑2024, including data from the American College of Obstetricians and Gynecologists, show a 1.5‑2% increase in bacterial vaginosis among copper IUD users compared with non‑IUD controls. Hormonal IUD users report a 3‑4% rise in candidiasis, mainly in the first year after insertion.
These numbers are still far lower than the infection rates seen with oral contraceptives that disrupt hormone levels systemically. The key takeaway: IUDs are safe for most women, but the type of device matters for specific infection patterns.
Comparing Copper and Hormonal IUDs: Infection Profiles
| Attribute | Copper IUD | Hormonal IUD |
|---|---|---|
| Primary infection type | Bacterial Vaginosis (≈1.8% increase) | Candidiasis (≈3.2% increase) |
| Biofilm propensity | Higher (copper surface attracts anaerobes) | Lower (levonorgestrel reduces bacterial adhesion) |
| Impact on Lactobacillus flora | Modest reduction | Minimal change |
| Typical duration | Up to 10years | 3‑7years (depending on brand) |
| Overall IUD infection risk | Low (≈2% cumulative) | Low (≈3% cumulative) |
When choosing a device, consider personal history. Women with recurrent BV may lean toward a hormonal IUD, while those prone to yeast infections might favor copper.
Risk Factors That Heighten Infection Chances
Not every IUD wearer will develop a problem. Certain factors tip the balance:
- Insertion environment: Non‑sterile settings or rushed procedures increase bacterial entry.
- Pre‑existing dysbiosis: Low Lactobacillus counts before insertion set the stage for BV.
- Antibiotic use: Broad‑spectrum antibiotics can wipe out protective flora, creating a niche for Candida.
- Smoking: Nicotine impairs mucosal immunity, making biofilm formation easier.
- Frequent douching or harsh soaps: Disrupts the natural pH, encouraging overgrowth of harmful microbes.
Addressing these factors-like quitting smoking before insertion or avoiding douching-reduces the baseline infection risk.
Recognizing Early Signs and When to Seek Care
Because IUD‑related infections often start in the vagina, early symptoms are familiar:
- Thin, gray‑white discharge with a fishy odor (classic BV)
- Thick, white “cottage‑cheese” discharge, itching, or redness (candidiasis)
- Painful urination or lower‑abdominal cramping that doesn’t resolve within a few days
- Fever or chills-possible progression to PID
If any of these appear within the first two weeks after insertion, contact a healthcare provider. Prompt treatment usually involves oral metronidazole for BV or fluconazole for yeast infections. For suspected PID, a combination of broad‑spectrum antibiotics is standard.
Preventive Strategies for IUD Users
Prevention is a blend of medical protocol and everyday habits:
- Choose a skilled clinician: Look for providers with documented IUD insertion experience and strict aseptic technique.
- Screen before insertion: A vaginal swab to assess microbiome health can identify women who might benefit from prophylactic probiotics.
- Maintain good genital hygiene: Wash with warm water, avoid scented products, and change underwear daily.
- Consider probiotics: Strains like Lactobacillus rhamnosus GR‑1 have shown efficacy in restoring healthy flora after antibiotics.
- Schedule follow‑up visits: A check‑up at 4‑6 weeks post‑insertion ensures the strings are in place and the uterus isn’t inflamed.
- Stay informed about symptoms: Keep a symptom diary for the first three months; note any changes in discharge or comfort.
These steps collectively keep the infection rate under 3% for most users, aligning with the safety profile reported in large cohort studies.
Management Options if an Infection Develops
When an infection is confirmed, treatment pathways differ based on the IUD type and infection severity:
- BV or mild yeast infection: Most clinicians treat medically without removing the IUD. A 7‑day course of metronidazole (BV) or a single 150mg dose of fluconazole (yeast) is typical.
- Recurrent infections: If BV or candidiasis recurs two or more times within six months, removal of the IUD may be advised, especially for copper devices prone to biofilm.
- Pelvic inflammatory disease: Immediate IUD removal is recommended, followed by a 14‑day IV antibiotic regimen (ceftriaxone+doxycycline). Later, a new IUD can be considered once the infection clears.
After any removal, patients should wait at least one menstrual cycle before reinserting a new device, allowing the uterine environment to reset.
Related Topics Worth Exploring
Understanding the IUD‑infection link opens doors to broader conversations:
- Contraceptive method comparison: How IUDs stack up against implants, pills, and condoms in terms of infection risk.
- Microbiome‑focused fertility care: The role of Lactobacillus dominance in successful pregnancies.
- Antimicrobial‑coated IUDs: Emerging technologies that embed silver or antibiotic particles to deter biofilm.
- Long‑term reproductive health: Tracking how repeated IUD use influences pelvic health over a decade.
Readers interested in any of these can look for follow‑up articles in the Health and Wellness section.

Frequently Asked Questions
Does an IUD increase the chance of getting a yeast infection?
Hormonal IUDs release levonorgestrel, which can slightly thicken cervical mucus and create a warmer vaginal environment. Studies show a 3‑4% rise in candidiasis, mostly in the first year. The increase is modest, and good hygiene plus occasional probiotic use usually prevent problems.
Can a copper IUD cause bacterial vaginosis?
Copper ions can attract anaerobic bacteria, leading to a small uptick-about 1.5‑2%-in BV rates compared with women not using an IUD. The risk stays low if the insertion is sterile and the user avoids douching.
Should I get my IUD removed if I develop an infection?
For mild BV or a single yeast infection, removal isn’t needed-antibiotics or antifungals work fine. If the infection is severe (PID) or keeps coming back despite treatment, doctors typically advise removal, treat the infection, and reassess contraception later.
How long after insertion can I expect to feel any side effects?
Most women notice cramping or spotting for the first 1‑3weeks. Vaginal discharge changes related to infection usually appear within the first two months. If symptoms persist beyond three months, it’s time to get checked.
Are there IUDs that reduce infection risk?
Emerging antimicrobial‑coated IUDs, especially those with silver or antibiotic layers, show promise in lab studies for preventing biofilm. They’re not widely available yet, but clinical trials are underway.




Cecil Mays
September 22, 2025 AT 05:40Just got my copper IUD last month and honestly? No issues yet 🙌 But I’ve been taking probiotics daily and avoiding soap down there-just water. Feels like my body’s thanking me. Also, no douching. EVER. That’s just asking for trouble. 🤓
Sarah Schmidt
September 23, 2025 AT 00:29Let’s be real-this whole IUD discourse is just another neoliberal medicalization of female biology. We’re conditioned to believe that our bodies are broken machines needing ‘insertion protocols’ and ‘biofilm surveillance.’ The real issue? Patriarchal medicine pathologizes normal microbial diversity. Why not just let the vagina be? It’s been managing for millennia without a T-shaped foreign object lodged inside it. 🤔
Billy Gambino
September 23, 2025 AT 12:56The biofilm dynamics here are fundamentally ontological. The copper IUD, as a metallic substrate, induces a non-equilibrium thermodynamic state in the vaginal microbiota-disrupting the homeostatic gradient maintained by Lactobacillus spp. This isn’t merely ‘infection risk’-it’s a microecological collapse mediated by anthropogenic intervention. The hormonal IUD, by contrast, operates via endocrine modulation, creating a more stable niche-albeit one that favors fungal opportunists. The real tragedy? We’re still treating symptoms rather than systemic dysbiosis.
Karen Werling
September 23, 2025 AT 23:13My friend had a copper IUD and got BV twice in 8 months. She switched to hormonal and hasn’t had a yeast infection since. She swears by the probiotic gummies too-like, the ones with L. rhamnosus. Not a miracle, but it helped. Also, she stopped wearing tight jeans. Small changes, big difference. 💕
STEVEN SHELLEY
September 24, 2025 AT 06:27THIS IS ALL A BIG PHARMA LIE. IUDs are designed to make women sick so they’ll buy MORE drugs. Did you know the copper is coated with something that triggers inflammation? They want you to get BV so you’ll buy metronidazole. And the hormonal ones? They’re just slow-release estrogen bombs. The CDC knows. The WHO knows. But they won’t tell you. Google ‘IUD biofilm coverup’-you’ll see the truth. I’ve got 7 years of medical records proving this.
Emil Tompkins
September 24, 2025 AT 23:58So what? You got a tiny metal thing shoved in your uterus and now you’re shocked you got a yeast infection? Newsflash: your body doesn’t like foreign objects. Ever heard of evolution? Maybe stop sticking shit in your vagina and try a condom. Or better yet-just don’t have sex. 🤷♂️
Kevin Stone
September 25, 2025 AT 13:15Interesting that the article doesn’t mention that IUD insertion without prior STI screening is essentially medical negligence. If you’re not testing for chlamydia and gonorrhea before placement, you’re just inviting PID. And yet, clinics still skip it. Lazy. Dangerous. Unacceptable.
Natalie Eippert
September 25, 2025 AT 19:15It's disgraceful that American women are being pushed toward these devices without proper education. In my country, we don’t just shove foreign bodies into women without consent. We have standards. We have ethics. Here? It’s all profit. No wonder infection rates are rising. This is cultural decay.
kendall miles
September 26, 2025 AT 01:19Did you know that the copper in IUDs can leach into the bloodstream? I read a paper from a NZ university that linked it to elevated serum copper levels and neurological symptoms. They’re calling it ‘IUD toxicity.’ No one’s talking about this. I’ve got my IUD out. My brain fog cleared in 3 weeks.
Gary Fitsimmons
September 26, 2025 AT 16:37I had a hormonal IUD for 5 years. Got one yeast infection, treated it, and never thought about it again. My doctor said if it’s not hurting, don’t stress. And honestly? She was right. I felt great. Just listen to your body and don’t panic over every little change.
Bob Martin
September 27, 2025 AT 08:56Oh wow, a whole article about how IUDs cause infections. Groundbreaking. Next up: ‘The Shocking Truth That Water Can Make Your Hair Wet.’
Sage Druce
September 27, 2025 AT 22:55If you're reading this and you're nervous about getting an IUD, please know you're not alone. I was terrified too. But I found an amazing provider who took 45 minutes to explain everything. She gave me a pamphlet, answered every question, and didn't rush me. That’s the kind of care we deserve. You got this. 💪
Tyler Mofield
September 28, 2025 AT 22:43It is imperative to underscore that the insertion of intrauterine devices constitutes a significant medical intervention requiring stringent adherence to aseptic protocols. Deviations from established clinical guidelines constitute a breach of the standard of care and may result in iatrogenic complications. Patient autonomy must be balanced with evidence-based practice.
Patrick Dwyer
September 28, 2025 AT 23:31For anyone considering an IUD: don’t just pick based on what’s trending. Talk to a reproductive endocrinologist who specializes in microbiome health. I work with one who does pre-insertion vaginal swabs and tailors recommendations. It’s not covered by insurance everywhere, but it’s worth it. Knowledge is power.
Bart Capoen
September 29, 2025 AT 12:21my doc said i should wait 2 weeks after insertion before having sex. i did. no issues. also i switched to cotton undies. weird how simple stuff works. also i use coconut oil as lube. no weird smells. just saying.
luna dream
September 30, 2025 AT 00:22The IUD isn’t the problem-it’s the patriarchy. The fact that we’re even having this conversation means we’ve accepted that women’s bodies are battlegrounds for corporate medicine. They profit from your discomfort. They profit from your fear. They profit from your silence. Wake up.
Linda Patterson
September 30, 2025 AT 16:42Women today are so weak. Back in my day, we didn’t whine about yeast infections. We just dealt with it. IUDs are fine. If you can’t handle a little discharge, maybe you shouldn’t be sexually active. This is why America is falling apart.
Jen Taylor
October 1, 2025 AT 09:11Just wanted to say-thank you for writing this so clearly! I’ve been researching for months and this is the first thing that made sense. I’m getting a hormonal IUD next week and I’m nervous, but now I feel like I know what to watch for. Also, I bought L. rhamnosus probiotics from a local co-op. Fingers crossed!
Shilah Lala
October 2, 2025 AT 07:10Wow. So many words to say ‘sometimes IUDs cause infections.’ I could’ve just Googled ‘IUD side effects’ and saved 10 minutes. Thanks for the novel.
Christy Tomerlin
October 2, 2025 AT 19:17Copper IUDs are for people who like drama. Hormonal ones are for people who like to be weirdly dry. Pick your poison.