DPP-4 Inhibitor Joint Pain Risk Calculator
Understanding Your Risk
This tool estimates your potential risk of developing joint pain based on FDA data. It does not replace medical advice.
Your Risk Assessment
Key Findings
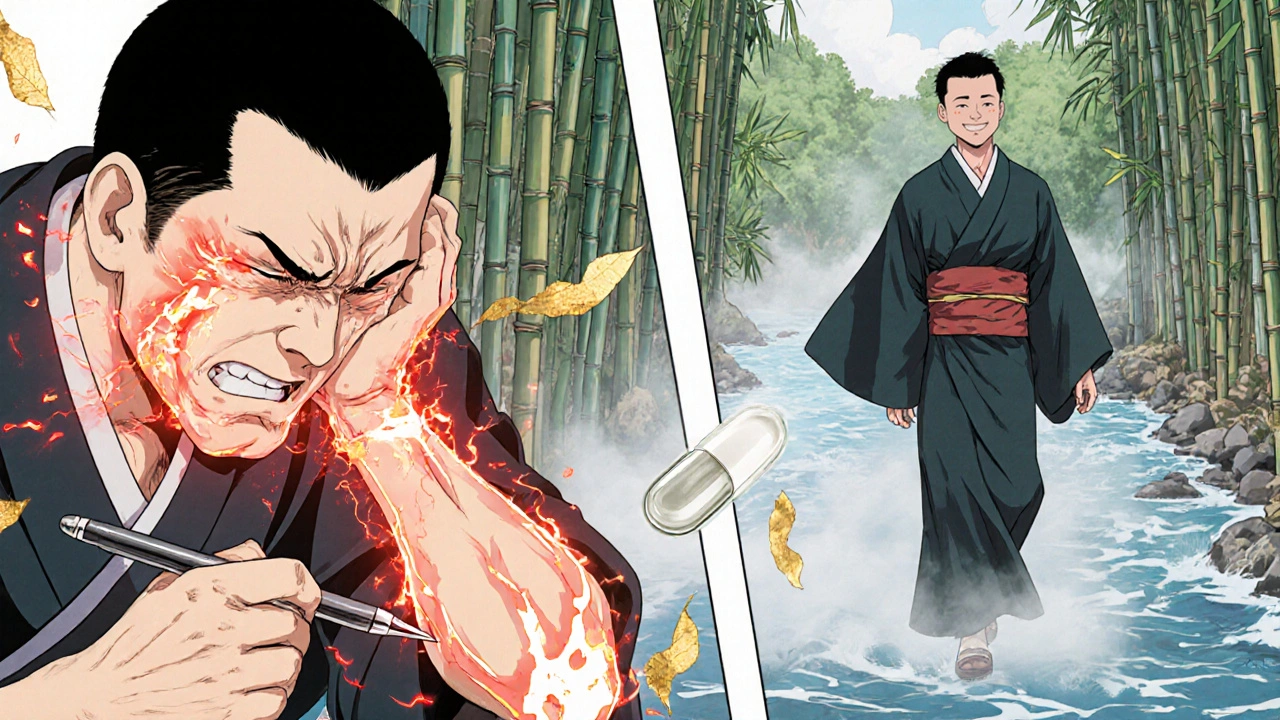
If you're taking a DPP-4 inhibitor for type 2 diabetes, and your knees, hips, or hands suddenly start hurting like never before, it’s not just bad luck. It could be your medication.
What Are DPP-4 Inhibitors?
DPP-4 inhibitors are oral diabetes drugs that help lower blood sugar by boosting natural hormones that tell your body to release insulin and stop making too much glucagon. They’re not insulin. They don’t force your pancreas to pump out more insulin all the time. Instead, they help your body use what it already makes - more efficiently.
Common names include sitagliptin (Januvia), saxagliptin (Onglyza), linagliptin (Tradjenta), alogliptin (Nesina), and vildagliptin (Galvus). These are some of the most prescribed diabetes pills in the U.S., with sitagliptin alone filling over 35 million prescriptions a year. For many people, they work well - low risk of low blood sugar, no weight gain, and easy to take once daily.
The Joint Pain Problem
In August 2015, the U.S. Food and Drug Administration (FDA) dropped a bombshell: DPP-4 inhibitors could cause severe, disabling joint pain. Not just a little ache. Not just after a long workout. Real, constant, movement-limiting pain that made people unable to walk, work, or even get out of bed.
The FDA reviewed over 7 years of reports - from 2006, when the first DPP-4 inhibitor hit the market, through the end of 2013. They found 33 clear cases where patients developed severe joint pain after starting one of these drugs. Twenty-eight of those cases involved sitagliptin. Five involved saxagliptin. Others were linked to linagliptin, alogliptin, or vildagliptin.
What’s chilling is how consistent the pattern was:
- 22 patients developed pain within a month of starting the drug.
- Some didn’t feel it until after a full year - meaning even long-term users aren’t safe.
- 10 patients were hospitalized because the pain was so bad.
- 23 of the 33 patients got better within a month of stopping the drug.
- 8 patients had the pain come back within days of restarting the same medication.
That last part is critical. When symptoms return after re-exposure, it’s not coincidence - it’s causation. The FDA called it "strong evidence" that the drug was the trigger.
Who’s at Risk?
It’s not clear why some people get it and others don’t. There’s no known genetic marker, no age cutoff, no weight threshold. The FDA reports included patients from their 40s to their 80s. Some had no history of arthritis. Others had mild osteoarthritis that suddenly turned into something far worse.
One case involved a 58-year-old woman who started sitagliptin and within three weeks, her knees swelled up and hurt so badly she couldn’t climb stairs. She thought she’d developed rheumatoid arthritis. Her doctor ran tests - nothing. Then she stopped the drug. Two weeks later, the pain vanished. When she accidentally took it again - within 48 hours, the pain returned.
That’s not rare. Multiple patients in the FDA database had the same story: misdiagnosed with autoimmune diseases, treated for lupus or gout, even referred to rheumatologists - only to find relief after stopping their diabetes pill.

How Common Is This?
It’s not common - but it’s real. The FDA says severe joint pain is rare, but that doesn’t mean it’s negligible. Out of 35 million prescriptions a year, 33 confirmed cases might sound tiny. But think about this: how many cases went unreported? How many patients just assumed their aching joints were "part of aging"? How many doctors didn’t connect the dots?
A 2021 study using real-world data from over 250 million Americans found that people taking DPP-4 inhibitors had a 24% higher risk of needing medical care for joint pain compared to those on other diabetes drugs. Another study of older veterans showed a 17% increased risk of joint pain among users. These aren’t lab results - they’re real people, real pain, real visits to the ER.
On the flip side, a large Taiwanese study found no link. But that study relied on hospital coding systems that often miss vague symptoms like "joint discomfort" unless it leads to a formal diagnosis. That’s a big blind spot.
What Does the Pain Feel Like?
It’s not the dull ache of arthritis. It’s deeper. Throbbing. Constant. Often bilateral - meaning both knees, both hips, both wrists. It doesn’t improve with rest. It doesn’t respond to ibuprofen. It wakes you up at night. People describe it as "my bones are on fire" or "like my joints are being crushed."
It can show up in any joint - shoulders, ankles, fingers. One patient reported pain in his jaw so bad he couldn’t eat. Another couldn’t hold a pen. A third had to quit her job because she couldn’t stand for more than five minutes.
And here’s the kicker: it can start at any time. You could be on the drug for 3 weeks. Or 3 years. There’s no safe window.
What Should You Do?
The FDA doesn’t tell you to stop. They say: Don’t quit cold turkey. If you’re having severe joint pain, call your doctor. Don’t wait. Don’t assume it’s just aging. Don’t self-diagnose.
Your doctor should consider DPP-4 inhibitors as a possible cause - even if you’ve been on them for years. They’ll likely ask you to stop the drug temporarily to see if the pain fades. If it does, and comes back when you restart it, the link is almost certain.
Most patients recover fully within a month of stopping. No long-term damage. No need for surgery. Just stop the drug, and the pain fades.
But if you stop without talking to your doctor, your blood sugar could spike. That’s dangerous. So work with your provider. They can switch you to another medication - metformin, SGLT2 inhibitors, GLP-1 agonists - and still keep your diabetes under control.
Other Side Effects to Watch For
Joint pain isn’t the only risk. DPP-4 inhibitors have been linked to:
- Pancreatitis - inflammation of the pancreas, which can be life-threatening.
- Severe allergic reactions - swelling of the face, lips, tongue, or throat.
- Bullous pemphigoid - a serious skin condition that causes blisters and peeling.
- Nausea, diarrhea, headache, stuffy nose - mild, but common.
If you develop blisters, swelling, or sudden abdominal pain, call your doctor immediately. Don’t wait.
Should You Be Afraid?
No. DPP-4 inhibitors are still a safe and effective option for millions of people with type 2 diabetes. The benefits - better blood sugar control without weight gain or low blood sugar - outweigh the risks for most.
But awareness matters. If you’ve been on one of these drugs and your joints started hurting, don’t ignore it. Don’t brush it off. Don’t assume it’s just "getting older."
Check in with your doctor. Ask: "Could this be my medication?"
It’s not about fear. It’s about knowing what your body is telling you - and having the power to listen.
Can DPP-4 inhibitors cause joint pain even after years of use?
Yes. While many cases of joint pain start within the first month of taking a DPP-4 inhibitor, the FDA has documented cases where symptoms appeared after a full year or more. This means even long-term users aren’t immune. If you’ve been on one of these drugs for years and suddenly develop new, unexplained joint pain, it’s important to consider the medication as a possible cause.
How do I know if my joint pain is from my diabetes medication?
There’s no single test. But if your pain is severe, persistent, and doesn’t respond to typical arthritis treatments, and it started after beginning a DPP-4 inhibitor, it’s worth investigating. The strongest clue is improvement after stopping the drug - and return of pain if you restart it. Your doctor may ask you to pause the medication temporarily to see if symptoms improve.
Will my joint pain go away if I stop the drug?
In most cases, yes. According to FDA data, 23 out of 33 patients experienced complete relief within one month of stopping the DPP-4 inhibitor. Pain typically fades gradually, not suddenly. Full recovery is common, and there’s no evidence of permanent joint damage from this side effect.
Are some DPP-4 inhibitors more likely to cause joint pain than others?
Sitagliptin (Januvia) was linked to the most cases in FDA reports - 28 out of 33. Saxagliptin followed with 5. But because the same pattern of pain, timing, and resolution occurred across all drugs in the class, the FDA considers this a class-wide risk. If you’re sensitive to one, you may be sensitive to others. Switching within the class isn’t recommended if joint pain occurred.
What are my alternatives if I need to stop a DPP-4 inhibitor?
Many options exist. Metformin remains the first-line treatment for most people with type 2 diabetes. SGLT2 inhibitors like empagliflozin or dapagliflozin offer heart and kidney benefits. GLP-1 receptor agonists like semaglutide or liraglutide are highly effective and can lead to weight loss. Your doctor will choose based on your overall health, other conditions, and insurance coverage.









Pradeep Kumar
October 30, 2025 AT 23:02This hit home for me. My dad was on Januvia for 2 years and suddenly couldn't walk without crying. Doctors thought it was arthritis, then gout, then "old age." We stopped the med on a hunch and within 3 weeks he was climbing stairs again. Never thought a diabetes pill could do this. Stay alert, folks 🙏
Pritesh Mehta
October 31, 2025 AT 14:51It's fascinating how Western medicine, in its infinite wisdom, continues to weaponize biochemical reductionism while ignoring the holistic integrity of the human organism. The DPP-4 inhibitors are merely symptomatic interventions, pharmaceutical Band-Aids on a systemic collapse fueled by industrialized diets and sedentary lifestyles. To blame the drug is to miss the point entirely - we are treating symptoms of a civilization in decline, not the disease itself. The joint pain? A metaphysical protest of the body against chemical interference in natural homeostasis. We must return to ancestral rhythms - not more pills.
Billy Tiger
November 1, 2025 AT 21:21Katie Ring
November 3, 2025 AT 09:08It's not about fear. It's about agency. You have the right to know your body is speaking - even if the language is pain. Too many people are told to endure, to wait, to assume aging is the culprit. But chronic pain that disappears when you stop the drug? That’s not aging. That’s a message. And we owe it to ourselves to listen - not just to doctors, but to our own lived experience.
Adarsha Foundation
November 4, 2025 AT 12:05Thanks for sharing this. I’ve seen patients in my clinic with exactly this pattern - misdiagnosed for months, then relief after stopping the drug. I always ask about new meds when joint pain pops up, but not every doctor does. Maybe we need a simple checklist: "Started new med? Pain bilateral? No trauma? Try stopping for 4 weeks." Simple, but it could save people a lot of suffering.
Alex Sherman
November 6, 2025 AT 05:16It's irresponsible to spread fear like this without emphasizing that the overwhelming majority of patients tolerate these drugs perfectly. People read headlines like this and panic - they quit their meds cold turkey, end up in the ER with DKA, and then blame the pharmaceutical industry. This isn't activism. It's medical malpractice by proxy. If you're not having symptoms, don't stop. If you are, see your doctor. Not Reddit.
John Concepcion
November 6, 2025 AT 21:36Caitlin Stewart
November 7, 2025 AT 00:11My sister had this. She was on saxagliptin for 18 months. Pain in both hips and wrists. Thought it was menopause. Went to three specialists. One finally asked if she’d started any new meds. She said yes - the diabetes pill. Stopped it. Two weeks later, she could hug her kids again. No scans. No surgery. Just stopped the drug. It’s not rare. It’s just ignored.